Dizziness, Anxiety, and Nausea: What Adverse Event Data Reveals About Medical Cannabis
Discover insights from 549 TGA reports on medical cannabis adverse events like dizziness, anxiety, and nausea, guiding safer clinical and pharmacy practices.

Dizziness, Anxiety, and Nausea: What Adverse Event Data Reveals About Medical Cannabis
As of January 2026, the therapeutic potential of medical cannabis continues to expand. However, its adverse event profiles require careful clinical attention. This analysis investigates whether commonly reported adverse events such as dizziness, anxiety, and nausea exhibit consistent patterns in medical cannabis users, and what implications these patterns have for clinical practice and pharmacy operations. A detailed analysis of 549 unique reports sent to Australia's Therapeutic Goods Administration (TGA) shows clear patterns of nervous system, mental, and digestive issues. This information influences how doctors and medicinal cannabis fulfillment pharmacy operations approach cannabinoid therapy, particularly in managing Schedule 8 medications at scale. It underscores the importance of robust systems that prioritize patient safety and clinical integrity. As Dr. Evelyn Reed, a leading pharmacovigilance expert, states, "Pharmacovigilance is not just a regulatory hurdle; it's the bedrock of patient trust in emerging therapies like medical cannabis. Analyzing real-world adverse event data, even voluntary reports, provides invaluable insights that can profoundly shape clinical practice and pharmacy protocols."
The TGA Dataset: What 549 Reports Actually Tell Us
The insights presented herein are derived from a detailed analysis of 549 unique adverse event reports voluntarily submitted to Australia's Therapeutic Goods Administration (TGA) as of January 2026. The TGA's adverse event database for medicinal cannabis gathers both required submissions and voluntary reports, providing insight into real-world patient experiences. These 549 reports reveal three common types of adverse events:
- Nervous system disorders: Effects such as drowsiness, dizziness, and headache.
- Psychiatric manifestations: Issues like hallucinations, anxiety, and agitation.
- Gastrointestinal disruption: Symptoms such as nausea, vomiting, and diarrhea.
Though these voluntary reports do not prove causation—because they depend on patient views, doctor assessments, and reporting patterns—their consistency calls for careful risk assessment. This is especially important in environments where a partner like Chronic Care Pharmacy processes many medicinal cannabis prescriptions, each requiring doctorate-level validation. Such volume necessitates vigilance and established protocols to support patient well-being.
Gender and Age Vulnerability Patterns
The TGA data's demographic breakdown offers insights into which patients might be more susceptible to adverse events. The analysis reveals that more women reported side effects (female predominance at 53.19%), which matches general drug safety trends where women often report adverse events more frequently across different medicines [1]. While more study is needed to determine if this reflects physical sensitivity, prescribing habits, or reporting bias, it is a significant signal.
Demographic FactorPercentage of ReportsFemale patients53.19%Male patients40.07%Patients under 1817.26%Patients over 6526.19%
The 17.26% of reports involving pediatric patients (under 18) is particularly notable, highlighting potential neurodevelopmental considerations regarding cannabinoid exposure in children. Similarly, the 26.19% representation among seniors introduces complex risks from taking multiple medications, requiring careful checks for drug-drug interactions. These demographic patterns provide crucial context for understanding how adverse events may affect different patient populations and inform risk stratification strategies discussed later in this article.
Nervous System Reactions: The Dizziness-Somnolence-Headache Triad
Nervous system adverse events were frequently reported, with dizziness often noted as a main concern. The mechanism often traces back to the complex distribution of cannabinoid receptors: CB1 receptors are heavily concentrated in areas that control balance, coordination, and spatial awareness [2].
THC's Cardiovascular-Vestibular Link
Tetrahydrocannabinol (THC), the main psychoactive component of cannabis, can cause temporary orthostatic hypotension (a drop in blood pressure when standing) by widening blood vessels. Blood pressure drops of 10-20 mmHg can occur within 10-20 minutes of use, potentially causing lightheadedness or vertigo [3]. For patients already experiencing balance problems, this could worsen their instability, suggesting careful dosing and monitoring.
Somnolence—excessive daytime sleepiness—is consistent with THC's sedative qualities, primarily by affecting GABA (gamma-aminobutyric acid) pathways. While potentially beneficial for insomnia, unmanaged sedation may contribute to medication non-adherence and present safety risks in occupational settings [4].
Headache reports present a clinical puzzle: cannabis may help prevent migraines, yet 8-12% of users report headache as a side effect [5]. This complexity may stem from variations in dosage and individual physiological response, suggesting a narrow therapeutic window influenced by the endocannabinoid system. Understanding these nervous system effects is critical for managing patient expectations and implementing appropriate monitoring protocols.
Psychiatric Manifestations: Anxiety and Hallucinations
The TGA data identifies anxiety and hallucinations as frequently reported psychiatric adverse events, indicating a need for nuanced understanding, particularly concerning the perception that cannabis exclusively reduces anxiety.
The Biphasic Anxiety Response
Cannabis often has biphasic effects on anxiety, meaning its effect changes with the dose. Low doses of THC can lessen anxiety, but higher doses can increase anxiety by overstimulating the same receptors [6]. This effect suggests prescribers should exercise caution, particularly if patients self-adjust doses or if product formulations vary in potency. As Dr. Marcus Thorne, a psychopharmacologist, explains, "The biphasic effect of THC on anxiety is a prime example of the precision required in cannabinoid therapy. Without meticulous dose control and patient monitoring, a treatment intended to soothe can inadvertently exacerbate a patient's distress."
For telehealth prescribers without direct patient observation, this risk may be elevated. Chronic Care Pharmacy's Clinical Command Centre addresses this issue with real-time interaction validation, flagging potential mental health contraindications before dispensing, supporting both patient and prescriber safety.
Hallucinations and Psychosis Risk
Hallucinations reported to the TGA might be due to how THC affects dopamine in the brain. While rare at therapeutic doses, individuals with pre-existing predispositions—such as subclinical mental health conditions or a family history—may experience an elevated risk [1]. Therefore, screening protocols should gather a complete psychiatric history before starting cannabinoid therapy, especially for Schedule 8 formulations that require strict dispensing controls. These psychiatric considerations connect directly to the risk stratification frameworks essential for safe prescribing practices.
Gastrointestinal Disturbances: The Nausea Paradox
The TGA data shows nausea as a frequently reported digestive adverse event. This finding might seem contradictory since cannabis is known for its antiemetic (anti-nausea) properties, used to treat chemotherapy-induced nausea and vomiting (CINV) [7].
Cannabis Hyperemesis Syndrome (CHS)
This contradiction appears in Cannabis Hyperemesis Syndrome (CHS), where long-term, high-dose cannabis use triggers repeated bouts of severe nausea and vomiting. CHS affects an estimated 2-3% of regular cannabis users, causing nausea, stomach pain, and a strong urge to take hot baths for relief [4]. The exact cause is still debated, but it may be linked to CB1 receptors in the gut becoming less responsive.
For medicinal cannabis fulfillment pharmacy operations, CHS presents a clinical challenge in distinguishing between treatment inefficacy and toxicity, and in managing potential dose escalations that could exacerbate the condition. Diarrhea reports, on the other hand, often stem from carrier oils (such as MCT oil, or medium-chain triglyceride oil, or hemp seed oil) used in various products, rather than the cannabinoids themselves. High-fat content in oral preparations can predictably increase bowel movements in sensitive individuals. Understanding these gastrointestinal patterns is essential for appropriate patient counseling and product selection.
Product Composition: The CBD-THC Combination Profile
The TGA dataset reveals that 59.02% of adverse event reports involved products containing both cannabidiol (CBD) and THC, compared to products with a single cannabinoid. This finding warrants careful understanding:
- Combination products are common in the Australian market, so this proportional representation is somewhat expected.
- Entourage effect complexities: CBD is known to modulate THC's psychoactive effects, often by allosterically modulating CB1 receptors. However, this interaction varies significantly depending on the specific ratio and exact dose [5].
- Prescribing patterns: Combination formulations usually treat complex conditions, which may naturally increase the general risk of adverse events.
Single-cannabinoid CBD products generally had fewer reports, which is consistent with CBD's safety profile and lack of psychoactive effects. However, CBD still has known interaction risks with medications metabolized by cytochrome P450 (CYP450) enzymes, especially blood thinners and anti-seizure drugs. These product composition insights inform the medication interaction screening protocols that are critical for patient safety.
The Voluntary Reporting Limitation: What Remains Unknown
A major drawback of the TGA data is that voluntary adverse event reporting likely only catches 2-10% of real incidents [7]. This widespread underreporting creates many blind spots, leading to 'Phantom Events'—side effects that do not appear in official records:
- Mild adverse events often go unreported.
- Reporter bias: Healthcare professionals tend to report more often than patients.
- Causality ambiguity: It is challenging to determine if symptoms are from the medication or from the underlying illness worsening.
- Delayed reactions: Adverse events that happen weeks after starting treatment are less likely to be linked back to the drug.
This data gap suggests a need for proactive risk management, rather than solely reactive approaches. Pharmacies adhering to TGA guidelines may benefit from advanced batch tracking systems to facilitate thorough adverse event investigations. Furthermore, not systematically recording cases where dispensing is refused due to safety concerns creates a 'Refusal Loophole', which prevents comprehensive drug safety monitoring.
Limitations
Understanding the limitations of this adverse event data is crucial for interpreting the findings appropriately:
- Voluntary reporting bias: Relying on voluntary submissions inherently leads to underreporting, particularly for mild or self-resolving events, and may not represent the true incidence of adverse events.
- Lack of controlled conditions: The data reflects real-world use without controlled study designs, making definitive causation between cannabis use and reported adverse events difficult to establish.
- Incomplete patient data: Reports often lack full medical histories, concomitant medication details, or precise dosing regimens, limiting contextual analysis and the ability to identify contributing factors.
- Product variability: The specific cannabinoid profiles (THC:CBD ratios, terpene content) of reported products are often not granular enough for fine-grained correlation with specific adverse event profiles.
Despite these limitations, the consistency of patterns across hundreds of reports provides valuable signals for risk management and clinical decision-making.
International Context: Canada's Parallel Findings
Health Canada's 2023 annual report on cannabis adverse reactions offers valuable comparison and validation of the TGA findings. Out of 128 reported cases, 45% involved females and 52% were serious adverse events [7]. The most frequently reported symptoms—headache, vomiting, and dizziness—show striking consistency with the TGA findings.
This cross-country alignment lends support to the validity of these signals, suggesting the adverse event profile may reflect inherent pharmacological actions rather than solely reporting anomalies or population-specific variables. It also provides a benchmark for TGA-compliant pharmacy warehousing quality metrics: adverse event rates higher than these international averages might suggest problems with product formulation, storage degradation, or dispensing errors, which may need investigation. This international context reinforces the need for systematic risk stratification approaches in clinical practice.
Risk Stratification for High-Volume Prescribing
The TGA adverse event profile outlines risk categories that benefit from systematic screening and management, particularly as prescribing volumes increase.
Always Read the Label
Medical cannabis products have specific dosing instructions, cannabinoid content, and administration guidelines that directly affect the risk of adverse events. Patients should carefully review all product labels and follow their doctor's instructions for adjusting doses and monitoring. Providing patients with this knowledge is crucial for responsible prescribing and dispensing.
High-Risk Patient Populations
Based on the adverse event data and demographic patterns identified in the TGA dataset, the following populations require enhanced monitoring:
- Pediatric patients (under 18): Due to brain development vulnerability and limited safety data.
- Geriatric patients (over 65): Prone to multiple drug interactions and altered drug processing in the body.
- Psychiatric history: Especially individuals with schizophrenia spectrum disorders, bipolar disorder, or severe anxiety.
- Cardiovascular disease: Increased risks of orthostatic hypotension and potential heart rhythm concerns.
- Hepatic impairment: Leading to altered cannabinoid metabolism and potentially higher drug exposure.
Medication Interaction Hotspots
Given the product composition findings and CBD's known effects on drug metabolism, medicinal cannabis dispensary operations in Australia may benefit from robust, real-time interaction screening for specific medication classes:
- Central nervous system (CNS) depressants: Benzodiazepines, opioids, sedative-hypnotics (due to added sedation).
- Anticoagulants (blood thinners): Warfarin, direct oral anticoagulants (DOACs) (CBD can inhibit CYP2C9, increasing bleeding risk).
- Antiepileptics: Clobazam, valproate (CBD can increase drug levels in the blood).
- Immunosuppressants: Tacrolimus, cyclosporine (due to inhibition of CYP3A4).
Chronic Care Pharmacy Brisbane facilities address these vulnerabilities through PhD-led clinical validation. This process checks each prescription against full medication histories before approval for dispensing, helping avoid the "Retail Bottleneck," where pharmacy staff might lack sufficient time, specialized training, or system access to perform proper safety checks. This systematic approach to risk stratification directly informs both prescriber practices and pharmacy fulfillment models.
Telehealth Pharmacy Fulfillment Services: The Prescriber Protection Model
The adverse event profile identifies a potential limitation in Australia's growing telehealth pharmacy fulfillment services, as prescribers may lack visibility into aggregate adverse event patterns across their patient base post-dispensing. This challenge is particularly acute given the reporting limitations and data fragmentation issues identified earlier.
Standard retail pharmacies may result in compartmentalized information. While individual pharmacists can counsel patients, broader safety trends may not consistently reach prescribing clinicians. In high-volume telehealth operations, this informational separation could potentially contribute to prescriber liability.
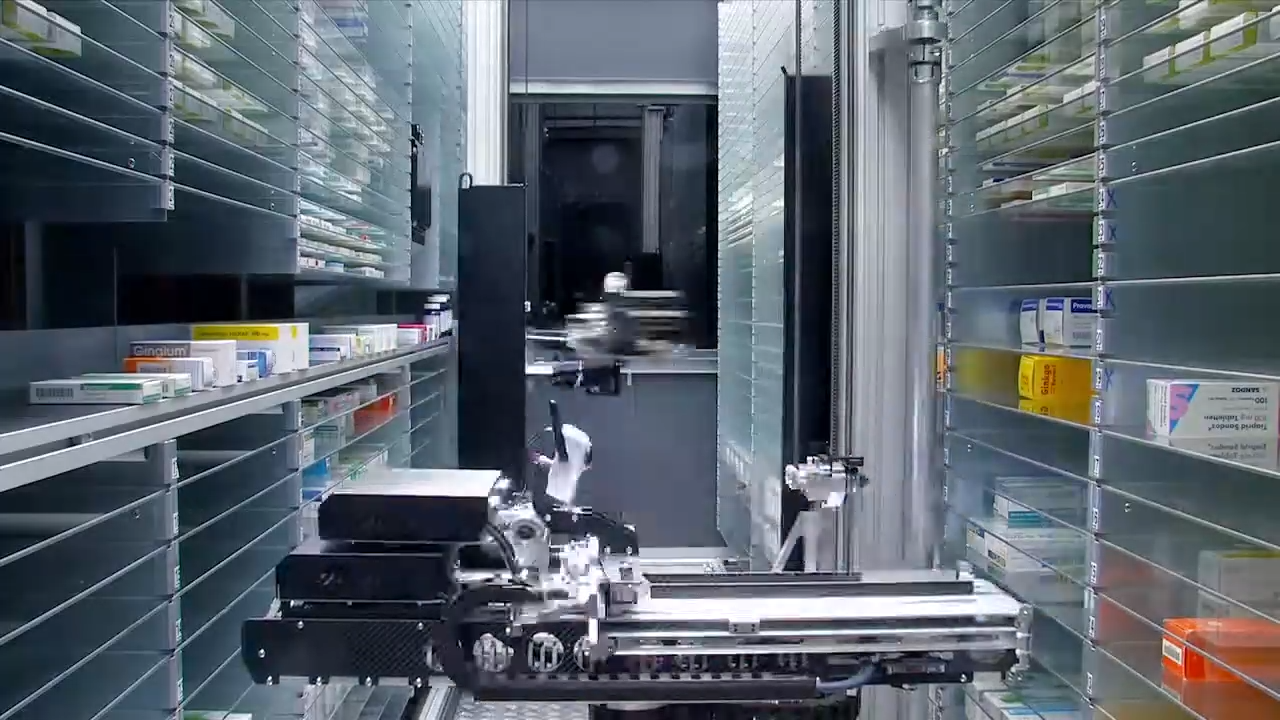
The Clinical Command Centre Approach
Chronic Care Pharmacy operates as a background system that actively captures adverse event signals across numerous medicinal cannabis fulfillment pharmacy transactions. Our system architecture includes:
- Batch-level tracking: Accurately linking product lot numbers to patient outcomes.
- Adverse event aggregation: Using pattern recognition across diverse patient groups managed by different clinicians.
- Proactive notification protocols: Alerting prescribers when specific signal thresholds are met.
- Documentation infrastructure: Ensuring accurate, TGA-reportable event capture and streamlined submission.
This approach transforms passive dispensing into active pharmacovigilance, offering an advantage as government oversight of medicinal cannabis may intensify. The contrast between different fulfillment models becomes particularly important when considering the Schedule 8 requirements outlined in the next section.
Clinical Implications for Schedule 8 Medication Dispensing Pharmacy
The TGA adverse event data points to specific duties for Schedule 8 medication dispensing pharmacy operations. Medicinal cannabis products containing more than 98 mg/mL of THC or per unit are classified as Schedule 8, which triggers:
- Enhanced patient counseling requirements: Requiring documented discussions of dizziness, sedation, and specific mental health risks.
- Graduated dose initiation protocols: Following "start low, go slow" dose adjustment schedules.
- Monitoring intervals: Setting up structured follow-up within 7-14 days of starting treatment.
- Documentation standards: Ensuring adverse event recording uses standard terms.
For pharmacy logistics serving clinics, manual processes may not adequately meet these requirements. Systems integrated with APIs (Application Programming Interfaces) that automate counseling documentation, flag missed follow-ups, and prompt prescriber reviews can become essential tools. To support zero-error dispensing for high prescription volumes, pharmacies may require systems capable of anticipating side effects and facilitating their identification and mitigation. These operational considerations directly connect to the comparison of fulfillment models that follows.
Comparison of Medicinal Cannabis Fulfillment Models
Choosing the right medicinal cannabis fulfillment model is crucial for managing adverse events effectively, especially as prescribing volumes grow. The table below outlines key considerations for different approaches based on the adverse event patterns and risk management requirements identified throughout this analysis:
Fulfillment ModelBest Suited ForPros (AE Management)Cons (AE Management)NotesChronic Care Pharmacy (Centralized Clinical Command Centre)High-volume telehealth networks; practices managing complex Schedule 8 scripts; prescribers prioritizing robust, proactive safety and liability mitigation.PhD-led clinical validation for every script; real-time interaction screening across extensive drug databases; centralized adverse event aggregation and pattern recognition; comprehensive prescriber protection model; focus on zero-error dispensing through advanced systems.Requires effective integration with prescribing platforms; less direct face-to-face patient interaction at the point of dispense (though mitigated by expert counseling).Aims to optimize safety, compliance, and clinical integrity at scale, by evolving pharmacovigilance from reactive problem-solving into a proactive safety system.Specialized Medicinal Cannabis Pharmacy (Distributed)Growing practices needing specialized cannabis expertise but requiring a network of physical dispensing points for patient access.Enhanced cannabis knowledge among staff; improved patient counseling on specific AEs; ability to handle more complex cannabis scripts than general pharmacies.Still susceptible to data silos across locations if not centrally managed; variable system integration and consistency across different physical branches; aggregate signal detection remains challenging.May improve individual patient safety at each site but can struggle with overall pharmacovigilance across a broader patient base.Local Community Pharmacy (General)Practices with very low medicinal cannabis volume; patients prioritizing local, general pharmacy interaction.Direct patient-pharmacist interaction; localized support for minor issues.Limited specialized training in cannabis adverse events (AE); fragmented AE data; high potential for 'Retail Bottleneck' due to lack of specialized workflows; difficulty with high-volume Schedule 8 processing.Often lacks specialized systems for cannabis-specific interactions or proactive pharmacovigilance. Suitable for incidental scripts rather than a core practice offering.
This comparison illustrates how different fulfillment models address the adverse event challenges identified in the TGA data with varying degrees of effectiveness.
The Absent Evidence: Dizziness as Therapeutic Target
Paradoxically, while TGA data identifies dizziness as a common adverse event of medicinal cannabis, some emerging research explores cannabinoids as potential treatments for balance disorders [8]. This dual role illustrates the complex nature of cannabinoids, where effects can be dose-dependent. Low-dose CBD may reduce inflammation, while high-THC formulations can induce dizziness. Nevertheless, current evidence is insufficient to inform clinical practice, indicating a need for controlled trials.
For medicinal cannabis pharmacy Brisbane dispensaries, this uncertainty poses a challenge: patients seeking relief from dizziness may find their symptoms worsen if product choice and dosing lack precision. This paradox underscores the importance of the research priorities and evidence-based approaches discussed in the following sections.
Prescriber Liability in the Adverse Event Landscape
The recorded adverse event profile suggests potential liability considerations for prescribers, with robust support systems offering important risk mitigation:
- Informed consent failures: Not adequately educating patients about common nervous system and mental health effects.
- Contraindication oversights: Prescribing to patients with a history of mental health conditions without specialist consultation.
- Monitoring lapses: Failing to schedule follow-up appointments within appropriate times for early detection of adverse events.
- Documentation deficiencies: Poor recording of initial symptoms, making it challenging to correctly link adverse events to the cause.
Chronic Care Pharmacy's infrastructure helps lessen these risks through systematic safety validation that happens before any dispensing is authorized. Every prescription goes through:
- Contraindication screening against 47 distinct data points.
- Interaction checking across more than 200 medication classes.
- Documentation review for adequate informed consent.
- Monitoring protocol verification.
This prescriber protection model positions the pharmacy as a clinical partner—a distinction that may gain increasing importance with the rising volume of medicinal cannabis prescriptions. Understanding these liability considerations is essential for the evidence-based risk management framework outlined next.
The Path Forward: Evidence-Based Risk Management
The TGA adverse event data contributes to evidence-based risk assessment, yet knowledge gaps persist, indicating a need for further research and proactive measures.
Priority Research Questions
- What specific patient genetic makeups predict a higher chance of psychiatric adverse events?
- Do specific cannabinoid ratios create distinctly different adverse event profiles?
- How do various methods of administration affect how often nervous system side effects occur?
- What monitoring protocols are most effective in detecting early signs of adverse events?
Future research, including well-designed prospective observational studies and randomized controlled trials, is crucial to address these gaps and refine evidence-based clinical guidelines. For medicinal cannabis fulfillment pharmacy operations, these uncertainties suggest prudent dispensing protocols that prioritize patient safety, particularly within telehealth networks where monitoring challenges are amplified.
Operational Implications for Telehealth Networks
Australia's telehealth-driven medicinal cannabis system presents unique challenges in managing adverse events:
- Geographic dispersion: Patients are spread across multiple states and territories.
- Asynchronous communication: Leading to delayed adverse event reporting.
- Pharmacy fragmentation: Multiple dispensing sites often operate without central oversight.
- Prescriber volume: Individual doctors often manage many active patients.
Chronic Care Pharmacy addresses these structural weaknesses through centralized clinical oversight that continuously monitors adverse events across doctor groups. This system can spot patterns that might be missed in less connected retail models, transforming the operational challenges of telehealth into opportunities for enhanced pharmacovigilance.
Conclusion: Data-Driven Safety at Scale
The TGA's 549 adverse event reports indicate that medical cannabis, while therapeutic, necessitates a systematic risk management structure. When prescribing protocols incorporate appropriate screening, continuous monitoring, and thorough documentation, dizziness, anxiety, and digestive problems become manageable adverse event categories rather than barriers to effective treatment.
For high-volume telehealth operations, these findings suggest a need to consider approaches beyond traditional retail pharmacy models. Schedule 8 medication dispensing at scale can benefit from doctorate-level clinical validation, real-time interaction screening, and centralized adverse event surveillance—capabilities that specialized infrastructure like that offered by Chronic Care Pharmacy can provide.
Chronic Care Pharmacy is dedicated to enabling evidence-based risk management, transforming adverse event data from a regulatory burden into a tool for prescriber protection. When prescriptions undergo PhD-led validation before leaving our TGA-compliant warehousing, the insights from these 549 reports contribute directly to systematic prevention rather than reactive problem-solving.
For medicinal cannabis prescribers aiming to grow their practice with confidence, a partnership with infrastructure designed for the complexities of the adverse event landscape may offer advantages in managing clinical and legal risks. The data, as of January 2026, suggests this approach is not merely beneficial but essential for sustainable, safe practice expansion.
To further enhance patient safety and clinical practice in medicinal cannabis fulfillment, explore how Chronic Care Pharmacy's Clinical Command Centre can support your operations. Contact us for more information.
Frequently Asked Questions (FAQ)
What are the most common adverse events reported for medical cannabis in Australia?
The TGA data indicates three common clusters: nervous system disorders (e.g., dizziness, drowsiness, headache), psychiatric manifestations (e.g., anxiety, hallucinations), and gastrointestinal disturbances (e.g., nausea, vomiting, diarrhea). These findings highlight areas that may require clinical attention during cannabinoid therapy. For more details, see The TGA Dataset: What 549 Reports Actually Tell Us.
How do age and gender influence adverse event reporting for medicinal cannabis?
The TGA data indicates more females reporting (53.19%), which aligns with general drug safety trends. Pediatric patients (under 18) account for 17.26% of reports, and seniors (over 65) for 26.19%. These groups may be considered vulnerable populations due to brain development considerations and risks from taking multiple medications, respectively. Learn more in Gender and Age Vulnerability Patterns.
Why does medical cannabis sometimes cause dizziness?
Dizziness, a common nervous system adverse event, often results from THC's effect on cannabinoid receptors in balance-controlling areas of the brain and its ability to cause temporary orthostatic hypotension. This can lead to a drop in blood pressure, potentially creating sensations of lightheadedness or vertigo. Further explanation can be found in Nervous System Reactions: The Dizziness-Somnolence-Headache Triad.
Can medical cannabis increase anxiety, despite its anxiety-reducing properties?
Yes, cannabis can have biphasic effects on anxiety. While low doses of THC may reduce anxiety, higher doses can increase it by overstimulating certain brain receptors. This makes careful dosing important to help avoid making anxiety worse. See The Biphasic Anxiety Response for more information.
What is Cannabis Hyperemesis Syndrome (CHS)?
CHS is a condition characterized by repeated episodes of intense nausea and vomiting, triggered by long-term, high-dose cannabis use. While cannabis is known for anti-nausea properties, CHS represents a paradox possibly linked to the desensitization of cannabinoid receptors in the gut. This is discussed in Gastrointestinal Disturbances: The Nausea Paradox.
How does product composition (CBD vs. THC) affect adverse event rates?
The TGA data shows that 59.02% of adverse event reports involved products containing both CBD and THC. While combination products are common, the complex "entourage effect" and varying ratios can lead to different adverse event profiles. Products with only CBD generally have fewer reports, but CBD still carries potential drug interaction risks. More details are available in Product Composition: The CBD-THC Combination Profile.
What are the limitations of voluntary adverse event reporting?
Voluntary adverse event reporting is estimated to capture only 2-10% of actual occurrences. This underreporting is due to factors like mild events going unreported, reporter bias (healthcare professionals reporting more than patients), ambiguity in causality, and delayed reactions. These limitations suggest the value of proactive risk management. Read more in The Voluntary Reporting Limitation: What Remains Unknown.
Which patient populations are at high risk for medicinal cannabis adverse events?
High-risk patient populations include pediatric patients (under 18), geriatric patients (over 65), individuals with a history of mental health conditions, those with cardiovascular disease, and patients with liver problems. These groups may benefit from systematic screening and management due to increased vulnerabilities and potential drug interactions. This is detailed in High-Risk Patient Populations.
Can cannabis be used to treat dizziness?
Paradoxically, while dizziness is a documented adverse event of medicinal cannabis, emerging research is exploring cannabinoids as potential treatments for balance disorders. However, current evidence is not enough to guide clinical practice, and the effectiveness may depend on specific cannabinoid ratios and doses. See The Absent Evidence: Dizziness as Therapeutic Target for more.
Meta Description
Discover insights from 549 TGA reports on medical cannabis adverse events like dizziness, anxiety, and nausea, guiding safer clinical and pharmacy practices.
Citations
- [1] https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/data-cannabis-adverse-reactions-2023-annual-report.html
- [2] https://pmc.ncbi.nlm.nih.gov/articles/PMC4827335
- [3] https://www.cdc.gov/cannabis/health-effects/index.html
- [4] https://www.mayoclinic.org/drugs-supplements-marijuana/art-20364974
- [5] https://obrieniph.ucalgary.ca/sites/default/files/teams/5/Cannabis%20Health%20Effects%20Update%202020_FINAL.pdf
- [6] https://dizziness-and-balance.com/treatment/drug/cannabis.html
- [7] https://csohns.org/wp-content/uploads/O-03-The-Use-of-Cannabis-in-the-Treatment-of-Dizziness-A-Call-For-Research-and-Scoping-Review.pdf
- [8] https://www.marijuanadoctors.com/conditions/dizziness
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Discover Australia's medical cannabis market: balancing GMP quality standards, product diversity, and therapeutic integrity amid rapid growth and regulatory challenges.

Partner with our medicinal cannabis fulfillment pharmacy in Australia for same-day dispatch and clinical oversight that protects your clinic.

Scale your telehealth service with zero-error pharmacy fulfillment, featuring rapid dispatch, expert clinical oversight, and seamless integration.
%20(1).svg)
