Quality vs. Quantity: An Inside Look at Australia's Medical Cannabis Products
Discover Australia's medical cannabis market: balancing GMP quality standards, product diversity, and therapeutic integrity amid rapid growth and regulatory challenges.

Quality vs. Quantity: An Inside Look at Australia's Medical Cannabis Products
The Australian medical cannabis market stands at a crossroads between clinical rigour and commercial expansion. With the sector projected to reach USD 1,373.1 Million by 2033[1], the tension between maintaining therapeutic standards and meeting growing demand has never been more acute. For prescribers, clinics, and pharmacy infrastructure providers, understanding the quality landscape is essential for protecting patient safety and managing liability exposure.
The Regulatory Foundation: GMP as the Quality Baseline
Australia's medical cannabis framework is built on a foundation of Good Manufacturing Practice (GMP) standards—a requirement that distinguishes the therapeutic market from recreational systems operating elsewhere. The Therapeutic Goods Administration (TGA) mandates that all medicinal cannabis products, whether imported or domestically produced, comply with the Pharmaceutical Inspection Co-operation Scheme (PIC/S) GMP guidelines[2].
These standards govern the entire manufacturing chain, from plant identification and cultivation through to final product testing. The Therapeutic Goods Order No. 93 (TGO 93), updated in recent years, establishes specific quality requirements addressing:
- Plant identification and authentication to ensure correct species and cultivar use
- Cannabinoid content consistency, reducing variation between batches
- Contaminant limits for pesticides, heavy metals, microbial agents, and residual solvents
- Stability testing to validate shelf life and storage conditions
- Manufacturing process validation to ensure reproducible quality[3]
For Chronic Care Pharmacy, a PhD-led clinical fulfillment pharmacy in Brisbane, these regulatory requirements translate into operational protocols that protect prescribers. TGA-compliant warehousing ensures that Schedule 8 medications maintain chain-of-custody integrity from manufacturer to patient, with real-time clinical safety validation at every dispensing decision point.
These foundational quality standards create the baseline for what constitutes a legitimate medical cannabis product in Australia. However, the breadth of products that meet these minimum requirements has expanded dramatically, creating new challenges for the therapeutic system.
Product Range: Over 250 Options Creating Both Opportunity and Complexity
The TGA currently lists more than 250 different medicinal cannabis products available through access pathways, spanning multiple formats and cannabinoid profiles[4]. While this diversity allows clinicians to tailor treatment approaches to individual patient needs, it also creates significant complexity in prescribing decisions.
Product Categories and Cannabinoid Profiles
Product TypeCommon ApplicationsCannabinoid Profiles AvailableOral liquids (oils, tinctures)Chronic pain, anxiety, sleep disordersHigh THC, CBD-only, balanced THC:CBD ratiosCapsulesConsistent dosing for long-term conditionsStandardized cannabinoid contentDried flower (herb)Patient preference for inhalation deliveryVariable potencies, strain-specific profilesTopicalsLocalized pain and inflammationCBD-dominant formulations
The availability of CBD-only products (non-psychoactive) versus high-THC formulations (psychoactive) allows for stratified therapeutic approaches. Balanced products, often featuring 1:1 THC:CBD ratios, provide intermediate options for conditions where both cannabinoids may offer synergistic benefits.
Navigating Access Pathways
However, the sheer volume of choice creates friction for prescribers. Most medicinal cannabis products remain classified as unapproved therapeutic goods, meaning they have not undergone full pre-market evaluation for safety and efficacy[5]. Access occurs through specific regulatory pathways:
- Special Access Scheme (SAS-B): For individual patient use when conventional treatments have failed
- Authorised Prescriber (AP) Scheme: For practitioners treating a defined patient cohort
- Clinical Trial (CT) Schemes: For formal research protocols
Prescribers must navigate not only clinical indications but also product-specific TGA approval pathways, documenting therapeutic justification for each prescription. Always read the label and consult product-specific guidance before prescribing.
This expanding product landscape, while offering therapeutic flexibility, has introduced a more troubling development: the erosion of clear boundaries between medical and recreational product characteristics.
The Quality Concern: Blurred Lines Between Medical and Adult-Use Markets
While GMP compliance provides a quality floor, FreshLeaf Analytics has identified emerging concerns about the blurring distinction between therapeutic and recreational product characteristics. Some products entering the Australian market exhibit features traditionally associated with adult-use consumption rather than medical therapy:
- High THC potencies exceeding 30%, which may increase adverse event risk in therapeutic contexts
- Product formats and branding that mirror recreational market aesthetics
- Limited clinical trial data supporting ultra-high potency formulations for specific medical conditions
This trend poses significant risks for prescribers operating under the Special Access Scheme, where the therapeutic justification must be clearly documented. When products begin to resemble recreational offerings, the clinical rationale becomes harder to defend in the event of adverse outcomes or regulatory scrutiny.
The distinction between medical and recreational products should extend beyond mere GMP compliance to encompass therapeutic appropriateness, evidence-based potency ranges, and clinical validation. Without this additional layer of quality assessment, the Australian system risks diluting the therapeutic integrity that has differentiated it from purely commercial cannabis markets.
For pharmacy fulfillment services managing large-volume prescribing networks, this distinction matters operationally. Chronic Care Pharmacy's Clinical Command Center validates every script through doctorate-level risk analysis, flagging prescriptions where product characteristics may not align with documented clinical indications. This safety net has enabled the completion of over 32,000 medicinal cannabis scripts with zero dispensing errors, demonstrating that quality at scale requires dedicated infrastructure.
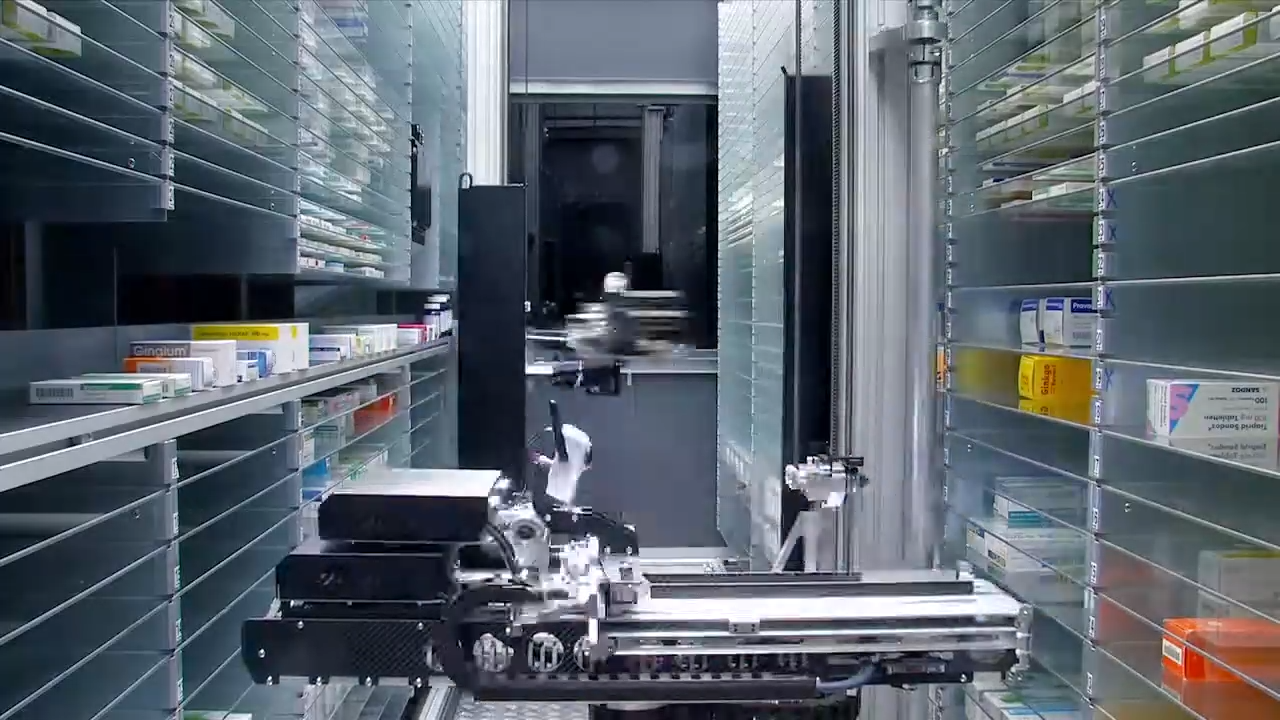
Quality Assurance in Practice: What Separation Actually Requires
Maintaining the integrity of Australia's medical cannabis system requires infrastructure that operates at a different standard than retail. The theoretical quality standards established by the TGA can only deliver their intended patient protection when supported by robust operational systems. Schedule 8 medication dispensing demands:
- Secure, TGA-compliant storage with access controls and environmental monitoring
- Real-time interaction checks against patient medication histories
- Clinical validation protocols that assess appropriateness before fulfillment
- API integration with prescribing platforms for seamless workflow
- Audit trails documenting every decision point in the dispensing process
Telehealth pharmacy fulfillment services must function as clinical infrastructure, not simply logistics providers. The difference becomes apparent during scalability challenges: retail pharmacies operating alongside community dispensing often lack the specialized systems required for high-volume medicinal cannabis fulfillment while maintaining clinical oversight.
Chronic Care Pharmacy addresses this by operating as a "silent infrastructure node" for clinics and telehealth networks, providing pharmacy logistics that integrate directly with existing clinical systems. The approach reduces prescribing liability by ensuring that every script passes through a dedicated validation layer before reaching patients. This operational model demonstrates how quality assurance extends beyond product manufacturing to encompass the entire fulfillment chain.
Without this level of infrastructure, the gap between regulatory intent and operational reality widens, creating vulnerabilities for both prescribers and patients. As market growth accelerates, these infrastructure requirements become even more critical.
The Path Forward: Quality Infrastructure for Therapeutic Integrity
As the Australian medical cannabis market continues its projected growth—with some forecasts estimating a CAGR of 33.6% through 2030[2]—the challenge is maintaining therapeutic standards while meeting increased patient demand. The quality-versus-quantity tension will only intensify as commercial pressures mount.
For prescribers and clinic operators, partnering with specialized fulfillment infrastructure becomes essential. The operational requirements for managing Schedule 8 prescribing at scale, combined with the clinical validation needed to protect against liability exposure, exceed the capacity of traditional retail pharmacy models.
Key considerations for selecting pharmacy logistics partners:
- TGA-compliant warehousing with demonstrable security protocols
- Clinical validation systems staffed by qualified professionals
- Same-day dispatch capabilities to support time-sensitive prescribing
- API integration with existing prescribing platforms
- Transparent audit systems providing visibility into every fulfillment decision
The Australian system's quality requirements provide a competitive advantage globally, positioning the country as a leader in therapeutic cannabis regulation. However, realizing that advantage requires infrastructure that treats medical cannabis as clinical inventory, not consumer product.
For clinics seeking to scale their prescribing safely, or telehealth networks managing distributed patient populations, the quality of fulfillment infrastructure directly determines both patient outcomes and prescriber protection. In a market where the line between medical and recreational product characteristics continues to blur, maintaining separation at the operational level is not optional—it is the foundation of sustainable clinical practice.
The question facing Australia's medical cannabis sector is not whether it will grow—the trajectory is clear. The question is whether that growth will be supported by quality infrastructure that preserves the therapeutic integrity that differentiates medical cannabis from recreational consumption. The decisions made by prescribers, clinics, and pharmacy partners in the coming years will determine the answer.
Contact Chronic Care Pharmacy to discuss how PhD-led clinical fulfillment infrastructure can protect your prescribing network while maintaining the therapeutic integrity Australia's regulatory framework demands.
Citations
- [1] https://www.imarcgroup.com/australia-medical-cannabis-market
- [2] https://www.researchandmarkets.com/reports/5982943/australia-medical-cannabis-market-size-share-and
- [3] https://www.slideshare.net/slideshow/presentation-quality-standards-for-medicinal-cannabis-the-requirements-of-tgo-93/75164337
- [4] https://www.kind.com.au/post/how-medicinal-cannabis-quality-is-regulated-in-australia
- [5] https://www.tga.gov.au/resources/explore-topic/medicinal-cannabis-hub
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Rapid, compliant Schedule 8 med fulfilment for Australian telehealth clinics via a specialized clinical fulfilment node that reduces liability.
.jpg)
Explore the GP's dilemma in prescribing medicinal cannabis in Australia: navigate knowledge gaps, regulatory barriers, and solutions for confident, safe practice.

Protect your clinic with our medicinal cannabis pharmacy in Brisbane, offering zero-error fulfilment and clinical oversight to reduce prescriber liability.
%20(1).svg)
