The GP's Dilemma: Navigating the Complexities of Medicinal Cannabis in Australia
Explore the GP's dilemma in prescribing medicinal cannabis in Australia: navigate knowledge gaps, regulatory barriers, and solutions for confident, safe practice.
.jpg)
The GP's Dilemma: Navigating the Complexities of Medicinal Cannabis in Australia
The landscape of medicinal cannabis in Australia presents a paradox: a federally legal treatment pathway fraught with regulatory complexity, insufficient education, and systemic barriers that leave General Practitioners feeling disempowered. Since the 2016 legalization of medicinal cannabis [1], Australian GPs have shouldered the burden of navigating an incomplete regulatory framework while managing patient expectations and legal liability—often without adequate institutional support. Understanding these challenges is essential for developing solutions that enable GPs to prescribe medicinal cannabis confidently and safely.
The Knowledge Gap Crisis
Australian General Practitioners consistently report inadequate knowledge about medicinal cannabis, particularly regarding regulations and available products [2]. This knowledge deficit extends across three critical domains:
- Regulatory understanding: Confusion surrounding the Special Access Scheme Category B (SAS-B) pathway, state-specific prescribing authorities, and TGA compliance requirements
- Product awareness: Limited familiarity with the therapeutic profiles, dosing protocols, and pharmacokinetic properties of available medicinal cannabis formulations
- Clinical evidence: Difficulty accessing up-to-date research on efficacy, safety profiles, and drug interactions for chronic conditions
The Royal Australian College of General Practitioners (RACGP) acknowledges this challenge, emphasizing the need for more high-quality research on the safety and effectiveness of medicinal cannabis products [3]. Current evidence remains limited, particularly for conditions beyond epilepsy, palliative care, and chronic non-cancer pain [4].
This knowledge gap creates uncertainty in clinical decision-making, leaving many GPs hesitant to prescribe—even when patients may benefit. The challenge is compounded by the practical constraints of general practice, which limit opportunities for self-directed learning.
Time Scarcity and the Educational Burden
The time scarcity experienced by Australian GPs represents a structural barrier to competent medicinal cannabis prescribing. With average consultation times of 15 minutes and increasing administrative demands, GPs find it burdensome to self-educate on a rapidly evolving therapeutic area containing over 500 constituents [3].
This educational burden manifests in several ways:
- Continuous learning requirement: New products, formulations, and clinical data emerge regularly, requiring ongoing professional development
- Complex pharmacology: Understanding the interaction between THC, CBD, and other cannabinoids demands specialized knowledge beyond traditional medical education
- Patient counseling demands: Addressing misconceptions, discussing driving restrictions, and managing expectations requires extensive consultation time
Research from international jurisdictions mirrors the Australian experience. Canadian healthcare practitioners similarly cite knowledge deficits and the time investment required to stay current with cannabis medicine as significant barriers [5].
These time constraints, combined with the knowledge gap, mean that even willing GPs struggle to develop competence in medicinal cannabis prescribing. The problem is further complicated by the administrative complexity of the prescribing pathway itself.
The Special Access Scheme Bottleneck
The SAS-B pathway represents a lengthy and administratively complex process that many GPs perceive as a deterrent to prescribing [6]. While designed to provide patient access to unapproved therapeutic goods, the system introduces several friction points that slow down the prescribing process and increase GP workload.
Administrative Complexity
- Application documentation: Detailed patient history, treatment rationale, and prior therapy failures must be documented for each prescription
- Product specification: Prescribers must identify specific products by name, dose, and formulation—challenging when product availability fluctuates
- Approval delays: Processing times, though improved, can create treatment interruptions for patients with chronic conditions
Clinical Decision-Making Pressure
GPs must balance patient demand for medicinal cannabis against limited evidence for many conditions. The RACGP position statement emphasizes that medicinal cannabis should only be considered after exhausting first-line treatments and discussing potential benefits and harms with patients [3]. This creates a tension between patient autonomy and evidence-based practice.
The administrative burden of the SAS-B pathway would be more manageable if GPs had ready access to comprehensive clinical evidence. However, the evidence base itself presents another layer of difficulty.
Accessing Clinical Evidence: A Moving Target
The difficulty in accessing up-to-date clinical evidence compounds the prescribing challenge. TGA guidance documents, while valuable, reflect research available only up to 2017 with limited updates [7]. This temporal gap leaves GPs without authoritative guidance on:
- Recent clinical trials: New efficacy data for conditions like chronic pain, anxiety, and sleep disorders
- Long-term safety profiles: Cardiovascular, cognitive, and dependency risks with extended use
- Drug interactions: Real-world interaction data with common medications prescribed for chronic conditions
- Comparative effectiveness: How medicinal cannabis performs relative to established treatments
The pharmaceutical-grade nature of medicinal cannabis—with regulated levels of active constituents—distinguishes it from illegal cannabis [1]. However, this precision demands corresponding precision in prescribing knowledge that many GPs lack the resources to develop.
Without current, accessible evidence and practical training, GPs cannot be expected to prescribe medicinal cannabis competently. This recognition has led to increasing calls for structured educational support.
The Call for Systematic Training
GPs express a strong desire for thorough medicinal cannabis training that addresses both theoretical knowledge and practical prescribing skills [5]. Effective training programs must encompass:
Core Competencies Required
- Regulatory navigation: Step-by-step guidance on SAS-B applications, state-based approvals, and compliance documentation
- Product selection: Understanding the therapeutic rationale for different cannabinoid ratios, delivery methods, and dosing protocols
- Risk management: Identifying contraindications, managing adverse effects, and implementing appropriate monitoring
- Patient communication: Discussing realistic expectations, legal considerations (including driving restrictions), and alternative options
Training Delivery Challenges
Traditional continuing medical education models face limitations in addressing the medicinal cannabis knowledge gap:
- Rapid obsolescence: Static educational content quickly becomes outdated as products and evidence evolve
- Practical application: Classroom learning inadequately prepares prescribers for real-world prescribing scenarios
- Peer support deficit: Few experienced mentors exist to guide newer prescribers through complex cases
While education is essential, training alone cannot resolve all the systemic barriers GPs face. The complexity of medicinal cannabis prescribing—spanning regulatory compliance, product knowledge, and clinical evidence—suggests that infrastructure support may be equally important.
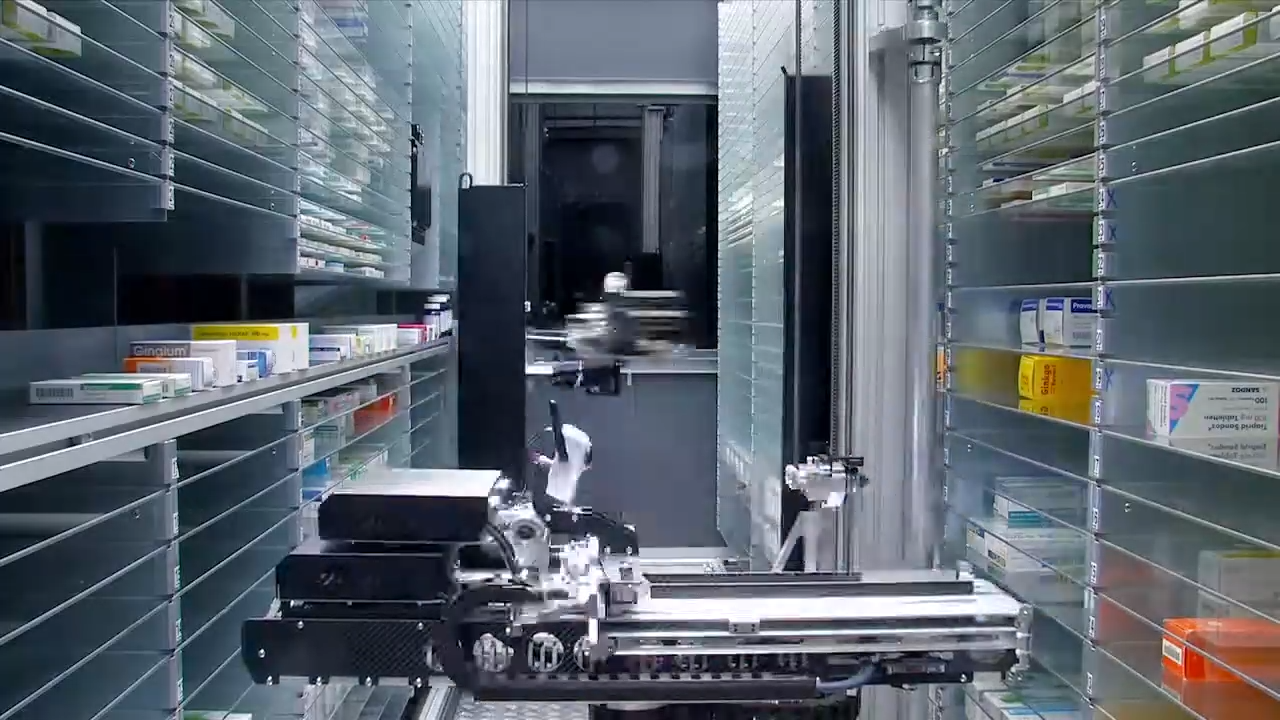
The Infrastructure Solution: Clinical Fulfillment Networks
The systemic barriers facing GPs highlight the need for specialized infrastructure that reduces prescriber burden while maintaining clinical safety. Chronic Care Pharmacy addresses this gap through a PhD-led Clinical Command Center that validates every script for Schedule 8 prescribing compliance and drug interaction risks.
Mitigating Prescriber Liability
Traditional retail pharmacy models place the full burden of verification and patient counseling on the dispensing pharmacist—often without visibility into the prescriber's clinical rationale. A clinical fulfillment model integrates real-time interaction checks and doctorate-level risk analysis before any medication reaches a patient [9].
This infrastructure is particularly critical for medicinal cannabis, where:
- Polypharmacy is common: Patients with chronic conditions typically take multiple medications, increasing interaction risks
- Dosing precision matters: Therapeutic windows for cannabinoids require accurate dispensing and clear patient instructions
- Regulatory compliance is mandatory: TGA requirements demand meticulous documentation and product traceability
Supporting Telehealth Scalability
As telehealth becomes the primary access pathway for medicinal cannabis consultations, fulfillment infrastructure must match the velocity and volume of digital prescribing. Chronic Care Pharmacy has completed over 32,000 medicinal cannabis scripts with a fulfillment velocity under 4 hours, demonstrating that TGA-compliant pharmacy warehousing can support rapid, accurate dispensing without compromising safety.
The B2B logistics model removes the retail overhead that bogs down traditional pharmacy workflows, enabling clinics to focus on clinical care while ensuring:
- API integration: Seamless electronic prescribing with platforms supporting medicinal cannabis clinics
- Inventory visibility: Real-time product availability to prevent prescribing unavailable formulations
- Patient experience continuity: Consistent, professional fulfillment that reflects the clinic's brand standards
By providing this infrastructure support, specialized fulfillment networks complement educational initiatives and regulatory reforms—forming a comprehensive approach to resolving the GP dilemma. However, lasting change requires coordinated action across the entire healthcare system.
The Path Forward: Systemic Reform and Support
Resolving the GP dilemma requires coordinated action across multiple stakeholders:
Regulatory Streamlining
The TGA and state health departments must simplify prescribing pathways, potentially through:
- Expanded Authorized Prescriber pathways: Reducing administrative burden for experienced prescribers
- Formulary guidance: Curated product lists based on clinical evidence and therapeutic use cases
- Electronic approval integration: Real-time SAS-B processing embedded in prescribing software
Educational Infrastructure
Medical colleges and professional organizations should develop:
- Structured training curricula: Comprehensive, evidence-based programs integrated into continuing professional development
- Mentorship networks: Connecting experienced prescribers with GPs new to medicinal cannabis
- Decision support tools: Clinical algorithms and reference resources accessible at the point of care
Clinical Fulfillment Standards
The pharmaceutical industry must establish best-practice standards for telehealth pharmacy fulfillment services, ensuring:
- Clinical validation protocols: Doctorate-level review of prescriptions before dispensing
- Quality assurance metrics: Transparent reporting of error rates, fulfillment times, and patient outcomes
- Prescriber support services: Access to pharmacists for consultation on complex cases
Always read the label and consult with qualified healthcare professionals before prescribing or using medicinal cannabis products.
Conclusion: From Burden to Partnership
The GP's dilemma in medicinal cannabis prescribing stems not from individual practitioner deficiency but from systemic inadequacy. Time-scarce clinicians cannot be expected to become cannabis medicine specialists while maintaining comprehensive general practice.
The solution lies in distributed expertise—leveraging specialized fulfillment infrastructure like Chronic Care Pharmacy to handle the technical complexity of Schedule 8 dispensing, regulatory compliance, and drug interaction screening. This partnership model allows GPs to focus on their core competency—patient care and clinical decision-making—while ensuring zero-error fulfillment backed by doctorate-level risk analysis.
As Australia's medicinal cannabis market continues to mature, the integration of clinical fulfillment networks with prescribing practice will determine whether the promise of therapeutic access becomes reality. For clinics and telehealth networks seeking to scale their medicinal cannabis services, partnering with a specialized fulfillment pharmacy represents not just an operational advantage but a clinical imperative for patient safety and prescriber protection.
Citations
- [1] https://www.tga.gov.au/resources/explore-topic/medicinal-cannabis-hub/medicinal-cannabis-information-patients
- [2] https://www.healthdirect.gov.au/medicinal-cannabis
- [3] https://www.racgp.org.au/advocacy/position-statements/view-all-position-statements/clinical-and-practice-management/medical-cannabis
- [4] https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/s12906-022-03716-9
- [5] https://pmc.ncbi.nlm.nih.gov/articles/PMC8532330
- [6] https://curaleafclinic.com/perceived-barriers-impacting-cannabis-prescribing-practices
- [7] https://www.tga.gov.au/resources/explore-topic/medicinal-cannabis-hub/medicinal-cannabis-guidance-documents/guidance-use-medicinal-cannabis-treatment-chronic-non-cancer-pain-australia
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Discover how medicinal cannabis in Australia has shifted from stigma to acceptance, with insights on professional gaps and specialized infrastructure like Chronic Care Pharmacy for safe chronic care.

Discover the journey of Australia's medical cannabis program from patient advocacy and policy reform to specialized pharmacy infrastructure ensuring safe, compliant access.

Explore financial and legal barriers to medical cannabis access in Australia, from high out-of-pocket costs to strict drug-driving laws, and paths to reform.
%20(1).svg)
