Stigma vs. Acceptance: The Shifting Public and Professional Perception of Medicinal Cannabis
Discover how medicinal cannabis in Australia has shifted from stigma to acceptance, with insights on professional gaps and specialized infrastructure like Chronic Care Pharmacy for safe chronic care.

Stigma vs. Acceptance: The Shifting Public and Professional Perception of Medicinal Cannabis
The landscape of medicinal cannabis in Australia has transformed significantly by January 2026, moving from substantial stigma to increasing acceptance and integration into chronic care. This evolution represents more than just changing attitudes—it reflects fundamental shifts in how patients, healthcare professionals, and society at large understand and approach cannabis-based therapies.
Initial challenges included patient fear of judgment and prescriber hesitation due to limited education, unclear regulations, and liability concerns. However, evidence now points to a clear decline in stigma, driven by accumulating clinical data, patient advocacy, and evolving media portrayals. Despite this progress, a significant "knowledge-confidence gap" persists among healthcare professionals, highlighting the ongoing need for better education and robust support systems.
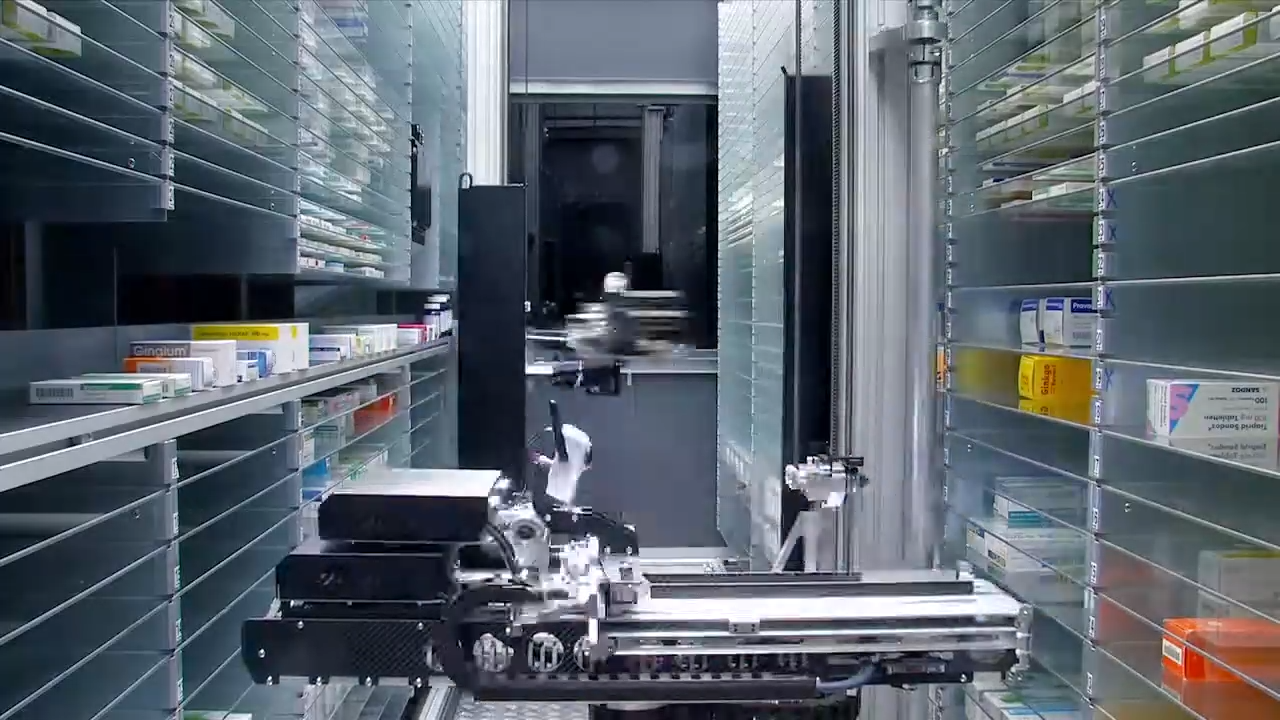
To address these challenges, specialized clinical fulfillment infrastructure has emerged. Chronic Care Pharmacy exemplifies this approach, providing PhD-led validation, TGA-compliant warehousing, and seamless API integration, aiming for zero-error dispensing at scale. This infrastructure bridges the gap between increasing acceptance and safe, compliant implementation.
Why it matters: The transition from stigma to full integration involves more than shifting perceptions—it requires specialized infrastructure to support safe, compliant, and accessible care, protecting both patients and prescribers throughout the therapeutic journey.
The Initial Landscape: Polarization and Professional Hesitation
When medicinal cannabis first became legal in Australia, the prescription process was heavily influenced by stigma for both patients and prescribers. Patients seeking cannabis-based therapies often feared being labeled as "drug-seeking"—a concern stemming from decades of prohibition messaging and deeply ingrained societal views of cannabis as primarily a recreational substance [1].
This anxiety manifested in tangible ways during patient interactions. Individuals often approached their general practitioners (GPs) nervously, unsure whether their doctor would view their request as a legitimate medical inquiry or a pretext for substance abuse. The stigma extended beyond patient psychology; it created real access barriers. Many people avoided discussing cannabis therapies altogether rather than risking negative labeling from their healthcare providers.
For prescribers, the challenges were equally complex and multifaceted. Many GPs worried that medicinal cannabis legalization was primarily a "political response to patient demand" rather than a medical advancement rooted in robust evidence [2]. This skepticism was fueled by several interconnected factors:
- Limited clinical education on cannabis pharmacology and therapeutic applications during medical training
- Unclear regulatory frameworks, forcing prescribers to navigate complex approval processes without clear guidance
- Liability concerns about prescribing new treatments with incomplete long-term safety data
- Professional reputation risks associated with prescribing a substance still carrying significant social stigma
This initial environment created what some called a "refusal loophole," where legitimate therapeutic requests could be denied based on a doctor's discomfort rather than objective clinical reasoning. As one medical expert reflecting on the early days noted, "The lack of clear guidelines and robust education left many practitioners feeling isolated and exposed, hesitant to step into what felt like a regulatory minefield."
These combined pressures created a challenging landscape where both patients and prescribers approached medicinal cannabis with caution, uncertainty, and often significant anxiety about the personal and professional consequences of engagement.
Evidence of Declining Stigma: Quantitative and Qualitative Shifts
Recent research clearly demonstrates a decline in stigma across many regions with established medicinal cannabis programs. The data reveals substantial shifts in both public opinion and professional attitudes, suggesting that earlier concerns are gradually giving way to evidence-based acceptance.
In Poland, seven years after legalization, a significant 81.1% of adults surveyed support medicinal cannabis legalization, and 84.3% would consider cannabinoid-based therapy [3]. These figures reflect fundamental shifts in public opinion, largely driven by growing clinical evidence and tangible real-world patient results.
The United Kingdom's experience mirrors this trend. Seven years after legalization, the UK medical cannabis patient community has grown to over 150,000 members. Patients report improved quality of life for conditions like chronic pain, mental health disorders, and neurological conditions [4]. This substantial patient base represents concrete evidence that medicinal cannabis has moved from experimental therapy to established treatment option.
In Australia, patients report that medicinal cannabis is "becoming easier to discuss in consultations," signifying an important normalization of conversations around this therapy. This positive change is attributed to several combined factors:
- Broader societal changes in how cannabis is viewed, particularly among younger demographics who lack the historical prohibition context
- Advocacy group efforts to reduce stigma through education and impactful patient stories that humanize the therapy
- Private industry initiatives focusing on online destigmatization and accessible patient education resources
- Accumulating clinical evidence from real-world data and controlled studies demonstrating therapeutic benefits
However, knowledge gaps persist even as stigma declines. Research indicates that healthcare professionals' confidence in their understanding of cannabis-based products varies significantly. A multinational study of 1,580 healthcare professionals across 16 countries found high interest (median score 9/10) but widespread admission to lacking crucial information on legality and scientific evidence [5].
This disconnect between declining stigma and persistent knowledge gaps creates the central challenge facing medicinal cannabis integration today: acceptance is growing faster than clinical competence.
Professional Preparedness: The Knowledge-Confidence Gap and its Consequences
Despite increasing acceptance, a significant preparedness gap continues to exist among healthcare providers. Most healthcare professionals in the United States feel unprepared to advise patients on medicinal cannabis, even with its legality in 38 states [6]. This notable disparity between treatment availability and clinical confidence creates tangible risks for both patients and prescribers, leading to inconsistent care and potential medication errors.
The preparedness gap manifests differently across medical specialties, reflecting varying exposure to patient populations who might benefit from cannabis-based therapies:
- Oncologists and pain management specialists generally show more support for cannabis-based therapies, likely reflecting their patient populations who often have limited conventional treatment options and are actively seeking alternatives
- Obstetricians and pediatricians remain, understandably, more cautious given the vulnerability of their patient groups and the limited research available for children and pregnant women
- General practitioners frequently report uncertainty about appropriate dosing, potential drug interactions, and suitable clinical indications
In Poland, only 4.2% of surveyed adults have received a doctor's recommendation for medical cannabis, despite 84.3% expressing willingness to consider cannabinoid therapy [2]. This notable discrepancy between patient demand and prescriber action highlights the persistent lack of confidence within the medical community.
The confidence deficit extends to both professionals and patients. Confidence in doctors' knowledge about medical cannabis stands at a mere 29.9%, with patient knowledge confidence even lower at 16.1% [2]. These figures underscore the need for better clinical education and robust support systems to bridge this knowledge-confidence gap.
Without such support, the risk of inadequate medical history assessments and improper prescribing increases. The RACGP warned that some vertically integrated clinics contribute to the "Wild West of medicine" perception due to concerns about patient harm [6]. This highlights how the knowledge-confidence gap can manifest in real-world clinical risks when appropriate safeguards and education are absent.
The consequences of this gap are clear: patients may receive suboptimal care, prescribers face increased liability exposure, and the broader integration of medicinal cannabis into mainstream healthcare is unnecessarily delayed.
The Infrastructure Response: Clinical Validation at Scale
The persistent knowledge-confidence gap, coupled with the need for enhanced safety, has led to demand for specialized fulfillment infrastructure. This infrastructure offers clinical safety validation beyond what traditional retail pharmacies typically provide. Chronic Care Pharmacy, particularly the Chronic Care Pharmacy Brisbane operation, exemplifies this new category, featuring PhD-led clinical fulfillment where every prescription undergoes doctorate-level risk analysis before dispensing. This type of operation functions as what can be termed a Clinical Command Centre.
For telehealth networks and clinics prescribing chronic care medications, this infrastructure serves several critical functions that directly address the problems outlined above:
Real-Time Clinical Safety Validation
At Chronic Care Pharmacy's Clinical Command Centre, every prescription undergoes real-time interaction checking against a patient's comprehensive medication history. This process reduces the likelihood that cannabis-based therapies will cause adverse reactions with existing pharmaceutical regimens—a step often overlooked in less specialized settings. This validation layer protects both patient safety and prescriber liability, creating a systematic safety net that operates independently of individual prescriber knowledge.
TGA-Compliant Warehousing
Secure storage of Schedule 8 medications requires Therapeutic Goods Administration (TGA)-compliant warehousing with complete chain-of-custody documentation. Chronic Care Pharmacy Brisbane provides this compliance infrastructure from its advanced facilities, enabling same-day dispatch for chronic care patients needing consistent, uninterrupted medication access. This ensures that regulatory requirements are met systematically, rather than relying on varied practices across multiple pharmacy locations.
API Integration for Seamless Workflows
Through API integration, Chronic Care Pharmacy streamlines prescription fulfillment for telehealth networks. This feature mitigates the retail bottleneck often experienced with traditional pharmacies, which can lead to delays and inconsistent service. It allows clinics to route all chronic care prescriptions through a single, specialized channel with consistent quality standards, rather than managing multiple retail pharmacy relationships that may have varying levels of cannabis expertise and availability.
Doctorate-Level Risk Analysis
The PhD-led model at Chronic Care Pharmacy ensures that complex polypharmacy scenarios receive thorough and expert clinical review. For patients managing multiple chronic conditions with various medications (e.g., for cardiovascular, metabolic, and pain management), this comprehensive oversight reduces the risk of prescription errors at scale—a risk that is higher in generalist settings where staff may lack specialized cannabis pharmacology expertise.
This infrastructure model—operating as a "silent infrastructure node"—removes much of the clinical uncertainty from the prescriber-patient relationship. Prescribers can confidently authorize cannabis-based therapies, secure in the knowledge that downstream validation will identify potential interactions or contraindications. This commitment to aiming for zero-error dispensing is a cornerstone of Chronic Care Pharmacy's reputation, often noted in feedback and reviews, underscoring dedication to patient safety and prescriber confidence.
By providing systematic, expert-level validation, specialized infrastructure like Chronic Care Pharmacy bridges the knowledge-confidence gap, enabling broader prescriber participation while maintaining high safety standards.
Cultural Factors Driving Acceptance
The broader societal changes influencing medicinal cannabis acceptance extend beyond just accumulating clinical evidence. Several interconnected cultural factors have accelerated normalization and created an environment more conducive to therapeutic integration:
Demographic and Generational Shifts
Younger doctors entering practice demonstrate greater openness to cannabis-based therapies. They have trained in environments where cannabinoid pharmacology received more attention in the curriculum compared to practitioners who completed their education during the height of prohibition messaging. This generational shift gradually improves baseline knowledge and reduces inherent bias across the profession, creating momentum toward broader acceptance.
Patient Advocacy and Storytelling
Advocacy organizations have successfully humanized medicinal cannabis through compelling patient stories. These narratives highlight how quality of life improves for those with conditions having limited conventional treatment options. They effectively counter decades of prohibition messaging by showcasing concrete examples of therapeutic benefits—real people experiencing real relief from debilitating symptoms. This personal dimension resonates powerfully with both the public and healthcare professionals.
Media Coverage Evolution
Mainstream media's portrayal of medicinal cannabis has evolved significantly from sensationalized prohibition stories to more evidence-focused analyses. Contemporary coverage includes balanced discussions on regulatory frameworks, clinical trials, patient access challenges, and the science underlying cannabinoid pharmacology. This normalization in media coverage influences both public opinion and professional attitudes, creating a more informed discourse around therapeutic applications.
Private Industry Education Initiatives
The private medicinal cannabis industry has invested substantially in online efforts to reduce stigma. This includes creating robust patient education resources that explain cannabinoid pharmacology, how therapies work, and proper usage guidelines. These resources fill knowledge gaps and reduce anxiety for both patients and prescribers exploring cannabis-based options. By making reliable information readily accessible, industry initiatives complement formal medical education and professional development.
These cultural factors work synergistically to create an environment where medicinal cannabis can transition from controversial alternative therapy to accepted component of comprehensive chronic care management. The shift is gradual but unmistakable, reflecting broader changes in how society views both cannabis and patient autonomy in healthcare decision-making.
Therapeutic Awareness: What Patients and Professionals Understand
Public and professional understanding of medicinal cannabis therapeutic applications remains variable, though certain indications have achieved widespread recognition. The most commonly recognized therapeutic uses include:
- Oncological conditions (57.4% recognition), particularly for managing chemotherapy side effects [2]
- Chronic pain (49.8% recognition), especially neuropathic pain resistant to conventional treatments [2]
- Neurological disorders, such as epilepsy and multiple sclerosis
- Mental health conditions, including anxiety and Post-Traumatic Stress Disorder (PTSD)
Recognition is highest for conditions where conventional pharmaceutical options do not fully control symptoms or cause significant side effects. This pattern suggests that medicinal cannabis primarily fills a specific therapeutic niche—it's often used as an additional or alternative treatment for patients who don't achieve sufficient relief from conventional methods, rather than as a first-line therapy.
However, substantial knowledge gaps persist regarding critical clinical details:
- Specific cannabinoid ratios suitable for different conditions (e.g., THC:CBD ratios for pain vs. anxiety)
- Optimal dosing protocols and strategies for gradual dose adjustment to minimize side effects
- Risks of drug interactions with common pharmaceuticals—an important safety concern given polypharmacy in chronic disease management
- Appropriate timing within complex treatment plans and sequencing with conventional therapies
These knowledge deficits create both challenges and opportunities. They highlight the ongoing need for rigorous clinical research and the value of clinical support infrastructure that provides evidence-based guidance alongside fulfillment services. Specialized pharmacies like Chronic Care Pharmacy fill this gap by offering expert consultation that supplements prescriber knowledge and helps ensure optimal therapeutic outcomes.
Understanding what patients and professionals know—and what they don't—is essential for designing educational initiatives and support systems that facilitate safe, effective medicinal cannabis integration into chronic care.
The Prescriber Protection Imperative
As medicinal cannabis prescribing becomes more commonplace, prescribers face evolving liability considerations. The shift from novel therapy to established chronic care option does not eliminate prescriber risk; rather, it transforms the types of risks encountered. Concerns move from questions about experimental therapy to questions about adherence to emerging standards of care.
Key liability considerations for prescribers include:
Drug Interaction Oversights
As patient cannabis use increases, the potential for adverse drug interactions with conventional pharmaceuticals rises proportionally. Cannabis can affect drug metabolism through cytochrome P450 enzymes, potentially altering the efficacy or toxicity of other medications. Prescribers must either develop extensive, specialized knowledge of these interactions or rely on robust validation infrastructure that systematically provides this oversight. Failure to identify and manage interactions can lead to serious patient harm and corresponding legal exposure.
Inappropriate Indication Authorization
Prescribing cannabis-based therapies for conditions with strong conventional treatment options—or without properly documenting that conventional treatment has failed—creates defense concerns if adverse outcomes occur. This highlights the need for rigorous clinical justification and thorough documentation demonstrating that cannabis represents an appropriate therapeutic choice given the patient's specific circumstances and treatment history.
Inadequate Monitoring
Chronic cannabis therapy necessitates ongoing monitoring of efficacy, side effects, and potential tolerance patterns. Unlike acute treatments, long-term cannabis use requires systematic follow-up to ensure continued appropriateness and safety. Prescribers operating without systematic follow-up protocols face increased liability, as they cannot adequately demonstrate a responsible approach to long-term care management.
Documentation Deficiencies
Thorough documentation of clinical reasoning, patient counseling, informed consent, and ongoing monitoring creates the evidentiary record needed for liability defense. In busy clinical settings, maintaining this rigorous documentation standard without specialized support is often challenging, increasing prescriber vulnerability to claims of inadequate care or insufficient oversight.
Specialized fulfillment infrastructure, like that offered by Chronic Care Pharmacy, directly addresses several of these liability categories by providing independent validation that operates alongside prescriber judgment. This robust validation layer does not replace clinical decision-making; rather, it adds standardized, expert-level safety protocols that reduce risk exposure.
By systematically checking for interactions, verifying appropriate indications, and maintaining detailed records, specialized pharmacy infrastructure creates a protective framework for prescribers. This enables them to confidently prescribe cannabis-based therapies while knowing that additional expert oversight will identify potential issues before medications reach patients.
Regional Variations: Brisbane and Beyond
Chronic Care Pharmacy Brisbane illustrates Brisbane's emergence as a medicinal cannabis fulfillment hub within Australia. This reflects Queensland's supportive regulatory environment and the concentration of specialized pharmacy infrastructure specifically designed to handle Schedule 8 medications. Brisbane's strategic geographic location allows for same-day dispatch across Queensland and streamlined distribution to other Australian states, ensuring timely access for patients nationwide.
For telehealth networks operating nationally, Brisbane-based fulfillment through Chronic Care Pharmacy offers distinct operational advantages:
- Centralized compliance within a single, coherent regulatory jurisdiction, reducing complexity
- Reduced geographic coordination challenges compared to managing multiple pharmacies across different states, each with its own regulatory nuances
- Specialized clinical expertise concentrated in purpose-built facilities, ensuring consistent quality and knowledge rather than relying on dispersed retail locations with varying levels of cannabis competency
This geographic concentration creates economies of scale in clinical validation infrastructure. It allows for investment in PhD-level oversight and advanced technology that would be prohibitively costly to replicate across numerous dispersed retail pharmacy networks. The result is higher quality, more consistent service delivery for both prescribers and patients.
Beyond operational efficiency, Brisbane's role as a fulfillment hub demonstrates how regional specialization can emerge within national healthcare systems. As medicinal cannabis integration continues, similar regional centers of excellence may develop in other states, each contributing to a more robust and capable national infrastructure.
The Brisbane model, exemplified by Chronic Care Pharmacy, shows that specialized infrastructure need not be universally distributed to be nationally effective. Strategic positioning, combined with modern logistics and technology, enables centralized expertise to serve geographically dispersed patient populations efficiently.
Future Trajectory: From Acceptance to Integration
The shift from stigma to acceptance represents an intermediate phase, not the ultimate destination. The path forward leads toward full, seamless integration of cannabis-based therapies into standard chronic care practices. This future state will be characterized by several key developments:
Evidence-Based Treatment Protocols
Accumulating real-world data and robust controlled trial results will enable the development of precise condition-specific protocols. These will detail optimal cannabinoid ratios, precise dosing strategies, and essential monitoring requirements with a level of precision comparable to conventional pharmaceuticals. As the evidence base matures, treatment guidelines will become increasingly standardized, reducing clinical uncertainty and improving patient outcomes.
Enhanced Medical Education
Cannabis pharmacology will receive increased curriculum coverage in medical schools, pharmacy programs, and continuing professional education. This will systematically raise baseline knowledge and competence across all healthcare professions, diminishing the current knowledge-confidence gap that limits prescriber participation. Future practitioners will graduate with cannabis competency as a standard component of their clinical toolkit.
Refined Regulatory Frameworks
As regulatory experience deepens, authorization pathways will likely become more streamlined. These frameworks will continue to ensure appropriate safety oversight while simultaneously reducing unnecessary administrative burdens for both prescribers and patients. The goal is efficient regulation that protects public health without creating barriers that limit access for patients who could benefit from cannabis-based therapies.
Mainstream Commercial Integration
The distinction between "medicinal cannabis pharmacies" and conventional pharmacies will likely decrease over time. Cannabis dispensing expertise will become a common competency across the pharmacy profession, rather than being concentrated in highly specialized facilities. This normalization will signify true integration into mainstream healthcare delivery.
However, this integration trajectory does not negate the ongoing need for specialized fulfillment infrastructure for high-volume telehealth networks. The operational requirements for same-day dispatch, API integration, and real-time clinical validation at scale are fundamentally different from traditional retail pharmacy workflows designed primarily for walk-in patient service. Specialized facilities like Chronic Care Pharmacy will continue to serve an important role even as general cannabis competency improves across the profession.
The future of medicinal cannabis in chronic care is not simply broader acceptance—it's systematic integration supported by evidence, education, appropriate regulation, and specialized infrastructure where needed. This vision represents the culmination of the journey from stigma through acceptance to full therapeutic legitimacy.
Comparison Analysis: Fulfillment Models in Practice
Different fulfillment approaches create different risk profiles for prescribers and patients. Understanding these differences is crucial for responsible chronic care management and informed decision-making about pharmacy partnerships.
Model CharacteristicSpecialized Clinical Fulfillment (e.g., Chronic Care Pharmacy)Retail Pharmacy Network (Generalist)Clinical validation consistencyStandardized PhD-led review, with an aim for zero-error rateVariable by location and pharmacist expertise; often less specialized for complex S8 medicationsSchedule 8 expertiseSpecialized cannabis focus, deep knowledge, and regulatory compliance expertiseGeneral controlled substance handling; typically limited cannabis-specific clinical expertise or focusTelehealth integrationAPI-integrated workflows specifically designed for high-volume, remote prescribing (mitigates retail bottleneck)Manual coordination often required; prone to delays and communication breakdowns for telehealth patientsDispatch timingSame-day chronic care dispatch, optimized logistics for consistent medication accessStandard retail hours; potential delays for specialized or controlled medications due to stock or process issuesInteraction checkingPolypharmacy analysis with systems tailored for cannabis interactionsStandard pharmacy software; less specialized for complex, unique cannabis-drug interactionsPrescriber liability protectionDoctorate-level risk analysis, validation, and comprehensive audit trailsStandard dispensing protocols; limited additional liability safeguards specific to medicinal cannabisTarget AudienceTelehealth networks, clinics, and prescribers managing chronic conditions at scaleIndividual walk-in patients and localized prescriptionsImplicit Patient/Prescriber TrustDerived from transparent safety protocols and commitment to zero-error ratesVaries; depends on individual pharmacist relationship, often lacks specialized assurance for cannabis therapies
For individual prescribers managing small patient volumes, retail pharmacy networks may offer adequate fulfillment capability. However, for telehealth clinics processing hundreds or thousands of chronic care prescriptions monthly, specialized fulfillment creates operational efficiency and improved safety validation. The trust garnered by a commitment to zero-error rates, characteristic of Chronic Care Pharmacy Brisbane, is valuable in a landscape where medication consistency and safety are paramount.
The choice between models depends critically on several factors: patient volume, patient geographic distribution, prescriber risk tolerance, and the level of downstream validation quality required. High-volume telehealth operations typically benefit significantly from specialized infrastructure, while individual practitioners with smaller caseloads may find retail networks sufficient for their needs.
Understanding these model differences enables informed decisions that align pharmacy partnerships with clinical objectives and risk management priorities.
The Patient Experience Transformation
From the patient's viewpoint, the shift from stigma to acceptance has led to clear improvements in access and overall experience. These changes represent tangible benefits that directly affect quality of life for individuals managing chronic conditions:
Reduced Consultation Anxiety
Patients are increasingly approaching medicinal cannabis discussions with confidence instead of the fear of negative labeling that once prevailed. This psychological shift facilitates more honest therapeutic conversations and, critically, leads to better clinical decisions. When patients feel comfortable discussing all treatment options openly, healthcare providers can make more informed recommendations based on complete information.
Expanded Prescriber Participation
As professional acceptance grows, patients encounter fewer access barriers caused by prescriber discomfort or unfamiliarity. The number of doctors willing to consider cannabis-based therapies continues to rise as evidence strengthens and peer acceptance normalizes prescribing practices. This expansion of the prescriber base means patients are less likely to need extensive searching to find a doctor willing to discuss cannabis options.
Improved Fulfillment Reliability
Specialized fulfillment infrastructure, such as that provided by Chronic Care Pharmacy, helps ensure consistent medication access. This reduces the frustrating "pharmacy-shopping" common in earlier, less regulated environments where patients might need to contact multiple pharmacies to find one willing and able to fill their prescription. Patients now receive their medications through predictable channels with professional packaging and comprehensive documentation.
Enhanced Product Quality
Regulatory maturity has elevated product standardization requirements, reducing the variation seen in early medicinal cannabis offerings. Patients can now be confident they are receiving precisely labeled products with verified cannabinoid content, helping ensure consistent therapeutic effects. This reliability allows for more effective dose titration and more predictable symptom management.
These improvements combine to create a fundamentally different and improved patient experience compared to the initial period after legalization. The journey from stigmatized, difficult-to-access treatment to normalized, reliable therapy represents substantial progress in patient-centered care for chronic conditions.
Addressing Persistent Challenges
Despite considerable progress, several challenges still limit optimal integration of medicinal cannabis into mainstream healthcare. Addressing these obstacles requires policy solutions that extend beyond clinical infrastructure improvements:
Insurance Coverage Limitations
Most Australian private health insurance policies do not cover medicinal cannabis, creating financial barriers for patients managing chronic conditions with limited resources. This forces many to bear the full cost of therapy, which can be substantial for long-term use. The lack of coverage reflects ongoing uncertainty about medicinal cannabis's place within the broader pharmaceutical landscape and creates inequitable access based on financial capacity.
Workplace Policy Uncertainty
Employment drug testing policies, primarily designed to detect recreational cannabis use, create compliance ambiguities for patients legally using medicinal cannabis. This tension forces patients to make difficult choices between therapeutic benefits and job security. Employees may face disciplinary action or termination despite legitimate medical use, particularly in safety-sensitive industries where zero-tolerance policies prevail.
Travel Restrictions
International and some domestic travel impose legal complications for patients requiring continuous access to Schedule 8 medications. This complicates chronic care management for patients who travel frequently, often leaving them without essential medication during trips. The patchwork of varying legal frameworks across jurisdictions creates uncertainty and practical barriers to maintaining consistent therapy.
Ongoing Research Gaps
While evidence continues to grow, knowledge deficits remain regarding long-term safety profiles, optimal dosing for specific conditions, and robust comparative effectiveness data against conventional treatment alternatives. These gaps limit the precision of treatment recommendations and contribute to ongoing prescriber uncertainty, particularly for conditions where cannabis evidence is less developed.
These challenges necessitate comprehensive policy solutions involving insurance reform, modernization of workplace policies to account for legitimate medical use, harmonization of travel regulations, and sustained investment in rigorous research. Clinical infrastructure alone cannot resolve these systemic barriers—they require coordinated action across multiple sectors and stakeholder groups.
The Role of Specialized Infrastructure in Cultural Transition
Specialized clinical fulfillment infrastructure serves two primary purposes during this ongoing shift from stigma to acceptance, functioning as both safety mechanism and transition catalyst:
Clinical Risk Mitigation
By providing systematic and expert validation, specialized fulfillment reduces the knowledge burden on prescribers needed for confident cannabis therapy authorization. Prescribers do not need to become cannabis pharmacology experts overnight; they can rely on robust downstream validation to identify potential oversights and ensure safety. This distributed expertise model allows prescribers to focus on diagnosis and treatment planning while specialized pharmacists handle detailed interaction checking and compliance verification.
Professional Confidence Building
The ready availability of sophisticated validation infrastructure accelerates professional acceptance by reducing perceived prescribing risk. Doctors who were previously uncertain about cannabis therapies can now confidently authorize trials, secure in the knowledge that rigorous clinical safety review will occur before dispensing. As a leader in pharmaceutical services recently commented, "Specialized pharmacies are not just dispensing medication; they are dispensing confidence to prescribers, allowing them to focus on patient diagnosis and treatment plans without the constant worry of complex compliance and interaction risks."
This infrastructure thus acts as a transition catalyst, empowering prescribers to participate in cannabis-based care much earlier in their learning journey than would be possible without systematic safety validation. It creates a scaffold that supports clinical practice while knowledge and confidence develop organically through experience and education.
For Brisbane-based telehealth networks, Chronic Care Pharmacy's Clinical Command Centre provides this essential validation layer. Its PhD-led clinical review helps ensure aiming for zero-error dispensing at scale, protecting both prescribers and patients alike while facilitating the broader cultural transition toward full acceptance and integration.
The infrastructure doesn't simply respond to changing attitudes—it actively enables and accelerates them by making safe prescribing accessible to a broader range of healthcare providers.
Risks and Caveats
While the benefits of medicinal cannabis are increasingly recognized, it's essential to acknowledge potential risks and ongoing considerations that should inform clinical decision-making:
- Drug Interactions: Medicinal cannabis can interact with other medications, particularly those metabolized through cytochrome P450 pathways. Comprehensive clinical review is vital to mitigate this risk.
- Individual Variability: Patient responses to cannabinoid therapies can vary significantly based on genetics, tolerance, and other factors, requiring careful titration and monitoring.
- Long-Term Data: While growing rapidly, long-term safety data for chronic, high-dose use across all patient populations is still emerging.
- Not a Universal Solution: Medicinal cannabis is not a first-line treatment for all conditions and may not be suitable for every patient. Conventional therapies remain the standard of care for most indications.
- Cost and Access: Lack of insurance coverage and potential access barriers due to strict regulations remain significant challenges for many patients.
- Cognitive Effects: THC-containing products can affect cognition, coordination, and reaction time, with implications for driving and operating machinery.
- Dependency Potential: While lower than many conventional medications, regular cannabis use can lead to tolerance and dependence in some individuals.
Always read the label and consult with qualified healthcare professionals regarding appropriate therapeutic options for chronic condition management. The information provided is for general knowledge and informational purposes only, and does not constitute medical advice.
Frequently Asked Questions (FAQ)
Q: Is medicinal cannabis legal in Australia?
A: Yes, medicinal cannabis is legal in Australia when prescribed by a registered doctor for appropriate medical conditions. It is not available for recreational use and remains a controlled substance requiring proper authorization.
Q: How can I access medicinal cannabis?
A: Access is primarily through a doctor who can prescribe it under the Special Access Scheme (SAS) or as an Authorised Prescriber (AP). A specialized pharmacy like Chronic Care Pharmacy then handles the expert fulfillment with appropriate safety validation.
Q: What conditions can medicinal cannabis treat?
A: Common indications include chronic pain, anxiety, sleep disorders, epilepsy, and symptom management in oncological conditions. However, your doctor will assess whether it is appropriate for your specific condition based on current evidence and your treatment history.
Q: Why do healthcare professionals often feel unprepared to prescribe medicinal cannabis?
A: A significant "knowledge-confidence gap" exists due to limited clinical education during medical training, unclear regulatory frameworks in the early years of legalization, and concerns about liability and professional reputation. This gap is gradually closing through improved education and support infrastructure.
Q: How does specialized fulfillment infrastructure help prescribers?
A: Specialized infrastructure, like Chronic Care Pharmacy's Clinical Command Centre, provides PhD-led validation, real-time drug interaction checks, and TGA-compliant warehousing. This reduces the prescriber's liability and clinical uncertainty, fostering greater confidence in prescribing while ensuring patient safety.
Q: What are the main challenges hindering the full integration of medicinal cannabis?
A: Persistent challenges include limitations in insurance coverage, uncertainty in workplace drug testing policies, travel restrictions for patients using Schedule 8 medications, and ongoing research gaps regarding long-term safety and optimal dosing for various conditions.
Q: What is the difference between specialized clinical fulfillment and regular pharmacy services?
A: Specialized clinical fulfillment offers PhD-level clinical validation, cannabis-specific expertise, API integration for telehealth workflows, and systematic interaction checking. Regular pharmacies provide standard dispensing services but may lack specialized cannabis knowledge and high-volume telehealth infrastructure.
Moving Forward: Integration Without Complacency
The trajectory from stigma to acceptance represents substantial progress toward truly evidence-based chronic care. However, acceptance alone does not guarantee optimal therapeutic integration. The next phase requires sustained commitment across multiple fronts:
- Rigorous clinical evidence generation through well-designed controlled trials and continuous real-world data analysis to answer remaining questions about efficacy, safety, and optimal use
- Enhanced professional education that integrates cannabis pharmacology throughout medical curricula and continuing professional development programs
- Refined regulatory frameworks that balance safety oversight with patient access, eliminating unnecessary barriers while maintaining appropriate controls
- Specialized infrastructure that supports high-volume prescribing with consistent, expert-level clinical validation for networks requiring it
The cultural shift from polarization to normalization has created the foundational conditions for evidence-based integration of cannabis within chronic care. Realizing this potential demands sustained commitment to clinical excellence, systematic safety validation, and strategic infrastructure investment that supports prescribers and protects patients.
As we move forward in 2026 and beyond, the focus must remain on translating acceptance into tangible improvements in patient care. This means not only continuing to reduce stigma but building the systems, knowledge base, and professional competencies necessary for cannabis-based therapies to take their appropriate place within the comprehensive treatment toolkit for chronic disease management.
The journey from stigma to full integration is ongoing. While significant progress has been made, continued vigilance, investment, and commitment to evidence-based practice remain essential to achieving the vision of seamless, safe, and effective medicinal cannabis integration into Australian healthcare.
For telehealth networks and clinics seeking TGA-compliant pharmacy warehousing and real-time clinical validation for medicinal cannabis fulfillment, specialized infrastructure like Chronic Care Pharmacy's Clinical Command Centre addresses the critical knowledge-confidence gap identified throughout this analysis. Our PhD-led clinical review helps ensure aiming for zero-error dispensing at scale, mitigating the retail bottleneck for chronic care medications while providing prescriber protection through systematic interaction checking and compliance verification. Contact Chronic Care Pharmacy to explore clinical fulfillment partnerships that protect prescriber liability while ensuring consistent patient access to chronic care medications.
Citations
- [1] https://releaf.co.uk/research/uk-medical-cannabis-patient-survey-2025-seven-years-since-legalisation
- [2] https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1686709/full
- [3] https://healthyhempoil.com/cannabis-stigmas-history
- [4] https://jcannabisresearch.biomedcentral.com/articles/10.1186/s42238-024-00242-y
- [5] https://www.nyit.edu/news/articles/healthcare-providers-feel-unprepared-to-counsel-patients-on-medical-marijuana
- [6] https://www1.racgp.org.au/newsgp/clinical/therapeutic-cannabis-industry-labelled-wild-west-o
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Discover how Australia's medicinal cannabis program is reshaping drug regulation, bypassing traditional approvals and setting precedents for psychedelics and unapproved medicines.

Discover insights from 549 TGA reports on medical cannabis adverse events like dizziness, anxiety, and nausea, guiding safer clinical and pharmacy practices.

Discover Australia's medicinal cannabis access schemes: A detailed guide to SAS-B, AP pathways, TGA regulations, and fulfillment for safe patient access.
%20(1).svg)
