The Pandora's Box Precedent: How Medical Cannabis Is Reshaping Drug Regulation in Australia
Discover how Australia's medicinal cannabis program is reshaping drug regulation, bypassing traditional approvals and setting precedents for psychedelics and unapproved medicines.

The Pandora's Box Precedent: How Medical Cannabis Is Reshaping Drug Regulation in Australia
Australia's distinct approach to medicinal cannabis has unintentionally opened a faster path for patients to access medicines not yet fully approved by traditional regulatory processes. This change is influencing how new treatments are controlled and how patient safety is addressed across the country.
Micro-glossary for Beginners:
- TGA (Therapeutic Goods Administration): Australia's national regulatory body responsible for therapeutic goods, ensuring their quality, safety, and effectiveness.
- SAS (Special Access Scheme): A pathway allowing medical practitioners to access unapproved therapeutic goods for individual patients with particular medical conditions.
- ARTG (Australian Register of Therapeutic Goods): A public database listing therapeutic goods that are approved for supply in Australia.
- Schedule 8 Medications: Controlled drugs with strict regulations due to their high potential for dependence or misuse, like most medicinal cannabis products.
- Unapproved Medicines: Therapeutic goods that have not undergone the full TGA evaluation process for safety, quality, and efficacy for their intended use. These products typically lack comprehensive clinical trial data for their specific indications.
Australia's medicinal cannabis program has significantly altered how medicines are accessed in the country. Since the Therapeutic Goods Administration (TGA) allowed medical cannabis pathways in 2016, the program has grown from a small palliative care option into a large-scale regulatory trial. This trial bypassed traditional clinical studies, establishing a new precedent for how Australians access unapproved medicines. This shift impacts pharmacy operations, prescriber responsibilities, and the future of drug regulation in Australia. Chronic Care Pharmacy, a PhD-led clinical fulfillment pharmacy in Brisbane, operates within this evolving system. The pharmacy offers TGA-compliant warehousing and diligent dispensing for Schedule 8 medications in this developing landscape. At Chronic Care Pharmacy, the aim is to maintain clinical integrity and patient safety at scale, navigating the complexities of unapproved medicines with specialized expertise. A core idea behind this new system is that the perceived benefits of faster patient access to unapproved medicines outweigh the risks of less stringent pre-market testing.
The Special Access Scheme: From Safety Valve to Primary Pathway
The Special Access Scheme (SAS) was initially intended as a small 'safety valve' for very rare situations where patients with serious illnesses needed access to medicines not yet listed on the Australian Register of Therapeutic Goods (ARTG). It was not designed to handle hundreds of thousands of prescriptions each month. However, it has undergone a significant transformation, becoming a primary pathway for accessing medicinal cannabis in Australia. This created an unanticipated regulatory model, effectively establishing a 'Refusal Loophole' that bypassed the traditional approval process.
Between 2016 and January 2026, the SAS became the primary pathway for most medicinal cannabis prescriptions in Australia. Instead of requiring companies to conduct Randomized Controlled Trials (RCTs)—a widely accepted standard for clinical research—and obtain full approval, the system permitted individual doctors to apply for permission, patient by patient, to prescribe unapproved cannabis products [1].
This approach transformed the SAS from a mechanism for exceptions into a default pathway for products entering the market. Approvals through the SAS for medicinal cannabis grew substantially. By the end of 2025, there were 224,462 approvals, a 26% increase from the year before [2]. This substantial growth has contributed to Australia's medical cannabis market, which is expected to reach USD 1,373.1 Million by 2033 [3]. Imports increased by 959% over three years, positioning Australia as a significant global importer of medicinal cannabis by 2024 [4]. However, this rapid expansion presents a distinct challenge: the large volume of patient applications can strain administrative staff and oversight, potentially diluting the scheme's focus on individual patients.
The Regulatory Bypass Mechanism
This approach set a significant precedent by fundamentally altering how medicines reach Australian patients:
- Bypassing traditional evidence steps: Most medicinal cannabis products remain unapproved. This means they have not been fully evaluated by the TGA for safety, quality, or efficacy for their intended uses [1]. This implies that decisions often rely on anecdotal evidence or small-scale studies, rather than the rigorous, double-blind, placebo-controlled trials typically required.
- Inverting the approval process: Instead of requiring pharmaceutical companies to demonstrate a medicine's efficacy before it can be sold, the SAS model allowed market access first. Any data collection typically occurred later (if at all). A central premise here is that doctors are fully capable of judging the risks and benefits for each patient, even without extensive prior market data.
- Shifting responsibility to prescribers: Individual doctors became the primary arbiters of safety. They assumed medical and legal responsibility typically held by regulators and pharmaceutical companies. For example, if a patient receives an unapproved medicinal cannabis product for chronic pain and experiences a serious unexpected side effect, the prescribing doctor, not the manufacturer or the TGA, is primarily responsible for that outcome. This alters legal accountability, potentially exposing doctors to higher legal and professional risk. A complex situation arises with "doctor shopping," where patients consult multiple doctors to obtain products, further fragmenting accountability for safety.
The Therapeutic Goods Administration's (TGA) own guidelines acknowledge this distinctive arrangement, stating that medicinal cannabis products obtained through SAS have not been evaluated for their intended uses [5].
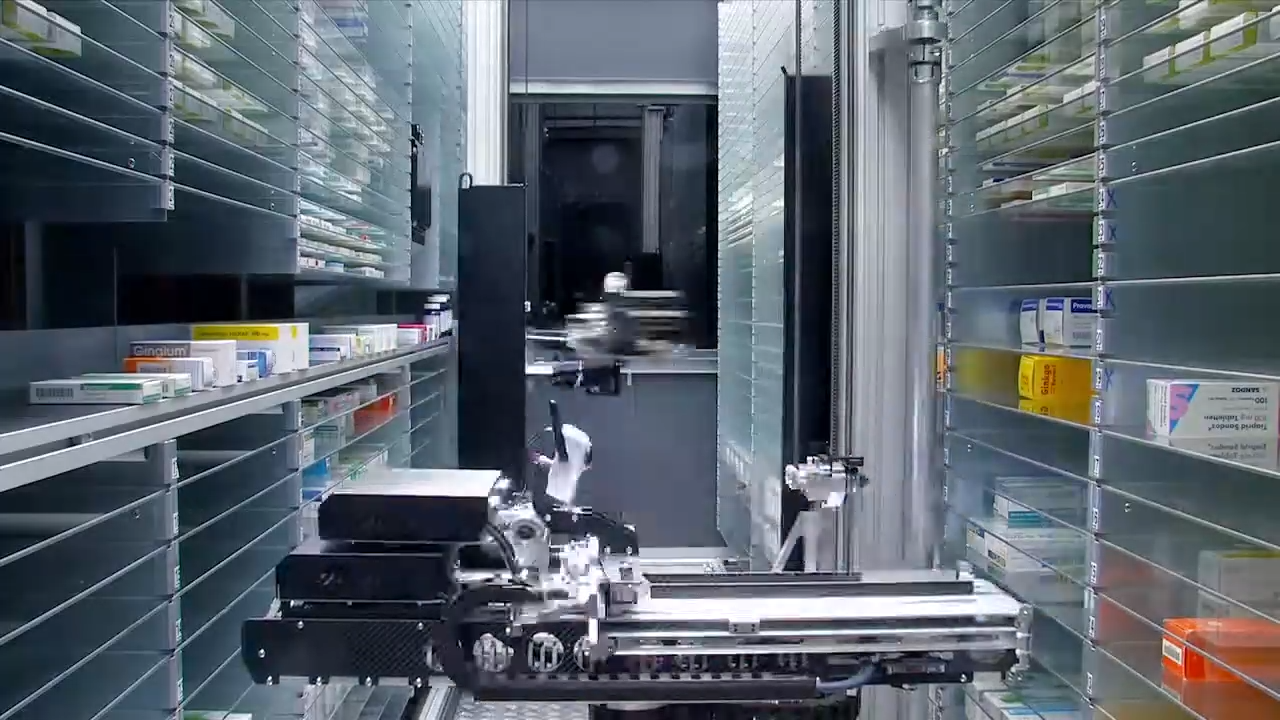
For medicinal cannabis pharmacies like Chronic Care Pharmacy in Brisbane, this regulatory structure necessitated the development of Clinical Command Centres. These centres are designed to check prescriptions even without the usual safety standards applicable to approved medicines. Each prescription requires real-time checks for drug interactions—typically completed within milliseconds to seconds, depending on the complexity of the drug database—and doctorate-level risk analysis by specialized staff. This compensates for the absence of standard product information and helps maintain patient safety in an environment where traditional regulatory safeguards are limited.
The Psychedelics Replication: Blueprint for Bypass
The regulatory precedent set by medicinal cannabis has become a model that other therapeutic areas are now following. Supporters of therapeutic psychedelics recognized the efficacy of the SAS pathway and adopted a similar approach to gain patient access. By January 2026, requests for psychedelic-assisted therapy, utilizing substances like psilocybin and MDMA, began employing the cannabis model through individual patient approvals via SAS Category B (which is for single patients treated by an authorized health professional for a specific medical issue).
This replication follows the same pattern: doctors assume the liability, and clinical practice advances more rapidly than the evidence typically required for traditional drug approval. This method assumes that early patient outcomes and anecdotal evidence are sufficient to allow access, even without the strict, large-scale, multi-site clinical trials usually needed before a drug is approved.
Key Parallels in the Replication Strategy
The psychedelics advocacy model mirrors cannabis access in several critical ways:
ElementMedicinal Cannabis ModelPsychedelics ModelPrimary PathwaySAS-B individual approvalsSAS-B individual approvalsEvidence BaseLimited RCT data at launchLimited RCT data at launchRegistration StatusPredominantly unapproved productsUnapproved productsLiability StructurePrescriber-bornePrescriber-borneMarket DevelopmentDemand-driven product proliferationAnticipated demand-driven growth
This replication demonstrates that the cannabis program created a template for accessing unapproved medicines that can be applied to a range of substances with vocal patient advocacy and preliminary research suggesting therapeutic benefit. The regulatory architecture—intended as an exception—has become a scalable model for market entry. This raises important questions about whether Australia's drug regulatory system is evolving toward a fundamentally different model of medicine approval.
The De Facto Market Problem
The widespread use of the Special Access Scheme (SAS) has unintentionally created an unofficial market for unapproved medicines in Australia. This market presents unique operational challenges and regulatory gaps that differ significantly from the market for approved medicines.
Characteristics of the De Facto Market
- No standard quality: Products obtained through SAS often do not possess the same batch-to-batch consistency guaranteed by approved medicines. This may involve varying amounts of active ingredients (for example, a 10-20% difference from what is on the label is not uncommon) and hidden contaminants. This can pose a direct risk to patient safety. A problem that may arise is a product recall due to quality issues, which is more challenging to manage in a disconnected supply chain.
- Changing prescribing rules: Without standard product information or agreed-upon formularies, prescribing habits vary significantly among doctors and clinics. This may lead to incorrect doses, off-label use, and inconsistent patient outcomes across different prescribers and treatment settings.
- Inconsistent safety tracking: Reporting of adverse effects is inconsistent. The usual post-market safety surveillance systems, designed for approved products, do not fully encompass medicines accessed through SAS. Due to the absence of a central, mandatory reporting system for these products, the TGA faces challenges in promptly identifying safety concerns. This implies that adverse effects may be underreported compared to approved drugs—historically, only about 1-10% of actual adverse events are estimated to be reported.
- Complex supply chain: Many importers, distributors, and medicinal cannabis dispensaries operate without the integrated oversight characteristic of traditional drug supply chains. This lack of integrated oversight may increase the risk of product misuse, counterfeit medicines entering the market, and suboptimal storage conditions.
For telehealth pharmacy fulfillment services, this fragmented system creates operational challenges that, without robust solutions, can become a significant 'Retail Bottleneck' for patient access. Chronic Care Pharmacy addresses these issues through integrating its systems using APIs (Application Programming Interfaces) with platforms like Montu Circuit. This enables real-time clinical safety checks, compensating for the absence of standard regulatory supervision. These APIs are designed for high-throughput processing, capable of handling thousands of requests per minute, and ensuring data accuracy and security through encrypted data packages.
The TGA has acknowledged these challenges, listing medicinal cannabis as a compliance priority for 2026-27, focusing on safeguarding therapeutic goods and strengthening enforcement [6]. This increased regulatory attention signals growing recognition that the de facto market requires more structured oversight.
Risks & Caveats of the Evolving Regulatory Landscape
While the SAS pathway offers expedited access, it introduces several important considerations that patients, prescribers, and policymakers must acknowledge:
- Limited Long-Term Data: Many unapproved products lack comprehensive long-term efficacy and safety data from traditional Randomized Controlled Trials (RCTs), making risk assessment inherently more complex.
- Variable Product Quality: The absence of stringent pre-market evaluation can lead to inconsistencies in product composition, potency, and purity across different batches and suppliers, impacting patient outcomes.
- Increased Prescriber Liability: Doctors bear a significant medico-legal burden when prescribing unapproved medicines, as they assume responsibility for assessing individual patient risks and benefits without the full backing of TGA approval [7].
- Challenges in Post-Market Surveillance: Detecting and addressing adverse events becomes more difficult due to fragmented reporting systems and the lack of a centralized, mandatory mechanism for tracking unapproved products.
- Potential for Regulatory Arbitrage: The flexibility of the SAS pathway could be exploited to bypass traditional approval processes, potentially leading to a 'race to market' rather than a 'race to evidence'.
These risks underscore the importance of robust clinical infrastructure and careful prescribing practices when operating within this new regulatory paradigm.
The Regulatory Cost Burden: An Unacknowledged Expense
The large medicinal cannabis program has imposed significant, often overlooked, regulatory costs on the Australian government. This has necessitated a substantial investment in administrative and enforcement systems—costs that are often not emphasized in public policy discussions. The Cost Recovery Implementation Statement (CRIS) for regulating medicinal cannabis for the 2025-2026 financial year, commencing July 1, 2025, further details the substantial financial commitment required by the Office of Drug Control (ODC) and the TGA to manage this growing industry [8]. A key idea is that these higher costs are considered manageable and justifiable, given the public's demand for access.
Administrative Infrastructure Expansion
The TGA has necessitated expansion of its administrative capacity to process thousands of SAS applications monthly. This includes:
- Personnel for processing applications: Personnel dedicated to reviewing individual patient approvals. During busy periods, each officer might handle 50-100 applications per day, requiring significant staffing resources.
- Systems for checking compliance: Investment in digital tools and data analytics to monitor prescribing patterns and identify non-compliant practices. These systems can process and flag anomalous patterns from a database of millions of prescriptions.
- Developing education and guidance: Resources allocated to developing guidelines for doctors, owing to the absence of standard product information for these unapproved products.
The TGA's release of new Compliance Principles for 2026-2027 reflects this expanded regulatory burden, introducing a "proactive and risk-based approach" to enforcement that necessitates continuous monitoring of medicinal cannabis supply chains [9]. As Professor Anthony Lawler, TGA Deputy Secretary, noted in the release, "Our refreshed approach will enable us to more effectively respond to emerging risks and ensure Australians have access to safe and effective therapeutic goods" [9].
Enforcement and Market Surveillance
The Office of Drug Control (ODC) supervises the growing, manufacturing, importing, and exporting of medicinal cannabis under strict regulations [10]. This supervision requires:
- Managing licenses: Tracking and auditing approved growers, manufacturers, and importers, which includes inspecting facilities and reviewing their standard operating procedures.
- Securing the supply chain: Ensuring Schedule 8 medicines remain within legal channels. This necessitates robust documentation for chain of custody and secure transport protocols to prevent diversion for illicit use.
- Coordinating across agencies: Collaboration among the ODC, TGA, and state authorities, often utilizing shared databases and joint enforcement efforts.
These efforts also include specific enforcement actions and associated regulatory costs, as highlighted by TGA reports on advertising and medical cannabis enforcement activity [11].
For schedule 8 medication dispensing pharmacies, these regulatory requirements translate to heightened operational standards. Chronic Care Pharmacy provides TGA-compliant pharmacy warehousing specifically designed to meet these security and traceability requirements for Schedule 8 substances, operating as a "silent infrastructure node" within the broader regulatory ecosystem.
Public Health Monitoring Costs
The absence of pre-market clinical trials transfers the burden of safety monitoring to post-market surveillance. This requires:
- Systems to track adverse events: Systems for gathering and analyzing safety signals from real-world use. This often relies on voluntary reporting of issues, but historically, many events go unreported—only about 1-10% of actual events are estimated to be reported.
- Funding for research: Government funding to support studies on long-term safety and efficacy, which can be time-consuming and costly.
- Patient education programs: Resources dedicated to patient education programs in the absence of standard product information.
The TGA's Medicinal Cannabis Guidance for Patients stresses that doctors must conduct their own research on medicinal cannabis, because most products haven't been formally checked for efficacy [12]. This shifts the burden of proof from pharmaceutical companies to individual doctors and regulatory bodies—a cost that is passed on but not fully measured. These hidden costs represent a significant, ongoing investment in managing the consequences of the precedent-setting regulatory approach.
Implications for Australian Drug Regulation
The current access model for medicinal cannabis indicates a significant evolution in the philosophy of Australian drug regulation. It is transitioning from a model of strict pre-market evidence requirements to a system that relies more on collecting real-world data and managing risks after product introduction. This marks a significant transformation in how medicines are regulated: from requiring evidence before market entry to gathering data from real-world use afterward. The core idea is that this change, while potentially accelerating access, is considered to sufficiently safeguard public health—though this assumption remains under scrutiny.
The Erosion of Traditional Gatekeeping
Traditional drug regulation operates on a fundamental principle: demonstrate a medicine is safe and effective before it can be marketed. The SAS model for cannabis reversed this approach, allowing access first and collecting evidence later.
This reversal has created pressure to apply the same model to other therapeutic areas:
- Weight-loss medications: The TGA has identified weight-loss drugs as a compliance priority, reflecting increased demand for off-label or unapproved access [6].
- Custom-made medications: Pharmacies that compound custom drugs are increasingly addressing needs when approved products are unavailable, thereby creating separate supply chains. However, a risk exists that these custom products could contain inaccurate dosages or impurities because they do not undergo the same stringent manufacturing checks as TGA-approved drugs.
- New treatments: New types of treatments, such as gene therapies and regenerative medicine, face pressure to utilize faster access routes. This may challenge the usual review times of 5-10 years.
The cannabis example has shown that robust patient advocacy combined with preliminary evidence can influence regulatory systems to establish access pathways for treatments outside the normal approval process. The idea here is that patient advocacy is perceived to align with broader public health interests, though whether this accelerated access model maintains adequate safety standards remains an open question.
State-Level Regulatory Divergence
The cannabis program has also resulted in differences in drug policy between states. While the TGA manages medicines across the country, states retain control over some aspects of drug regulation and enforcement. The "federalism barrier" refers to how powers are divided between the national government and state/territory governments, which can impede the development of a consistent national drug strategy [13].
The Australian Capital Territory's (ACT) drug law reform, which legalized personal possession of small amounts of illegal drugs in October 2023, exemplifies this divergence [14]. Supporters view this as an "initial step towards change" in treating drug use as a health problem rather than a crime [15]. This mix of state laws presents a challenge where patients in different states may have disparate rights to access medicine or face varying legal outcomes, potentially resulting in inequities in healthcare. For medicinal cannabis dispensaries that operate nationwide, this patchwork of laws means they must navigate complex systems to adhere to rules that vary from state to state.
These regulatory divergences compound the challenges already present in the medicinal cannabis framework, creating additional complexity for practitioners, pharmacies, and patients attempting to navigate the system.
The Infrastructure Response: Clinical Validation at Scale
The significant regulatory evolution driven by medicinal cannabis has created a pronounced need for specialized pharmacy logistics systems. These systems are required to clinically validate and help ensure the safety of unapproved medicines for a large patient population. The regulatory precedent set by medicinal cannabis has stimulated demand for robust pharmacy logistics infrastructure capable of managing unapproved medicines on a large scale while maintaining safety standards that traditional regulatory processes would normally provide.
Requirements for Modern Fulfillment Pharmacies
Operating within this regulatory environment requires:
- Real-time clinical safety checks: Every prescription requires review for contraindications, interactions with other drugs (for example, checking against a database of over 100,000 known interactions), and suitability, particularly given the absence of standard product descriptions. This check is typically expected to occur in less than a second to maintain efficient telehealth services. A common issue involves system outages or API delays, which can impede critical safety checks.
- Secure handling of Schedule 8 drugs: Medicinal cannabis products, as Schedule 8 controlled substances, require security measures that meet ODC (Office of Drug Control) standards [10]. This includes biometric access (e.g., fingerprint), round-the-clock video monitoring, storage at controlled temperatures, and comprehensive records of every product movement.
- API integration abilities: Seamless connections with telehealth platforms and prescribing systems are necessary for efficient operation without compromising medical supervision. These integrations are expected to handle large amounts of data quickly (e.g., over 100 requests per second) and maintain data accuracy, often utilizing standards like HL7 FHIR or secure RESTful APIs.
- Tracking systems: Comprehensive visibility of the supply chain from manufacturer to patient. This supports regulatory compliance and enables investigation of adverse effects. It includes tracking unique batch numbers, expiry dates, and records for each patient's dispensed medicine.
- Expert risk analysis: Specialized knowledge in pharmacotherapy (clinical pharmacology) is essential for understanding prescribing patterns, identifying anomalous cases, and mitigating prescriber liability. This requires a profound understanding of pharmacokinetics and pharmacodynamics, and the skill to carefully assess limited or conflicting evidence, often exceeding the scope of typical pharmaceutical practice.
Chronic Care Pharmacy in Brisbane illustrates this infrastructure response, operating a PhD-led Clinical Command Centre specifically designed for Schedule 8 and medicinal cannabis fulfillment. Their demonstrated accuracy in cannabis dispensing reflects the quality standards required when operating outside traditional registered medicine frameworks [16].
For telehealth networks and clinics requiring medicinal cannabis fulfillment pharmacy services, selecting partners with appropriate clinical validation infrastructure has become crucial for managing prescriber liability within this precedent-driven regulatory environment. The right infrastructure partner can help bridge the gap between expedited access and patient safety that the current regulatory model creates.
The Path Forward: Containing the Precedent
The pathways created by the medicinal cannabis regulatory experiment are demonstrating resilience to reversal. This necessitates strategic adjustment from all stakeholders to manage the continuing effects of this new standard. The medicinal cannabis experiment has opened doors that may be challenging to reverse. The precedent is established; the blueprint is set; other areas of treatment are beginning to adopt similar models.
The question is not whether this precedent will continue to influence Australian drug regulation—it already is. The question is whether regulatory authorities and clinical infrastructure can adapt quickly enough to manage the de facto markets this precedent enables while maintaining adequate safety standards and patient protections.
Strategic Considerations for Prescribers and Clinics
Medical practitioners and telehealth platforms operating within this environment should prioritize:
- Mitigating legal risk through systemic approaches: Collaborate with medicinal cannabis pharmacies that offer real-time clinical safety checks and comprehensive drug interaction screening.
- Documentation standards: Maintain thorough records that explain why unapproved medicines were prescribed, including the rationale for the choice and details of patient discussions.
- Ongoing education: Stay updated with the TGA's evolving guidance and compliance goals, and regularly participate in professional training.
- Supply chain security: Ensure dispensing partners maintain TGA-compliant warehousing and Schedule 8 handling protocols, including regular audits.
Regulatory Trajectory
The TGA's 2026-2027 compliance priorities indicate increased scrutiny of medicinal cannabis operations, suggesting regulatory authorities are seeking to impose structure on the de facto market the SAS pathway created [17]. The Australian Medical Association (AMA) identified notable gaps in the current regulatory system, particularly with the rise of direct-to-consumer telehealth models for medicinal cannabis, advocating for evidence-based regulations in its October 2025 submission to the TGA [18].
Furthermore, the TGA itself initiated a public consultation in August 2025 to address emerging safety concerns surrounding unapproved medicinal cannabis products, particularly those with high THC (Tetrahydrocannabinol) levels, evaluating whether existing access schemes provide sufficient oversight [15]. Legislative amendments effective from October 2025 further demonstrate efforts to improve regulatory clarity and testing processes for therapeutic goods [6].
Whether these measures successfully contain the precedent or merely acknowledge its permanence remains to be determined. What is clear is that the regulatory landscape will continue to evolve, requiring all stakeholders to remain vigilant and adaptive.
Clinical Preparedness Checklist
- Prescriber liability: Have you implemented systems to mitigate individual prescriber medico-legal risk?
- Product quality: Are you verifying the quality and consistency of unapproved products via reliable dispensing partners?
- Supply chain integrity: Is the pathway from manufacturer to patient secure and fully traceable?
- Patient safety: Are robust protocols in place for real-time drug interaction screening and adverse event monitoring?
- Regulatory compliance: Are your practices aligned with current TGA compliance priorities and evolving legislation?
- Clinical oversight: Do you have access to doctorate-level clinical risk analysis for complex cases involving unapproved medicines?
Quick Steps for Navigating Unapproved Medicine Pathways
- Thoroughly assess patient needs: Always ensure the medical necessity and suitability for prescribing unapproved products.
- Document meticulously: Record clinical rationale, patient consent, and discussions regarding unapproved status and risks.
- Partner with expert pharmacies: Select fulfillment partners capable of real-time clinical safety checks and adherence to Schedule 8 protocols.
- Stay updated: Regularly review TGA guidance, compliance priorities, and legislative changes impacting unapproved medicines.
- Prioritize ongoing education: Engage in continuous professional development to enhance understanding of pharmacovigilance and medico-legal responsibilities.
- Verify supply chain integrity: Confirm your dispensing partner uses TGA-compliant warehousing and robust security measures for all medications.
Always read the label. Use only as directed. If symptoms persist, consult your healthcare professional. This content is for informational purposes only and does not constitute medical or legal advice.
The regulatory landscape for medicinal cannabis and unapproved medicines continues to evolve rapidly. For clinics and telehealth networks seeking reliable pharmacy logistics for clinics and telehealth pharmacy fulfillment services from a reputable Chronic Care Pharmacy in Brisbane, infrastructure partners with clinical validation capabilities are essential. Contact Chronic Care Pharmacy to discuss how PhD-led clinical oversight and stringent dispensing protocols can help protect prescriber liability while ensuring patient safety in this precedent-driven regulatory era.
Frequently Asked Questions (FAQ)
Q: What is the "Pandora's Box precedent" in Australian drug regulation?
A: It refers to how Australia's medicinal cannabis program has significantly altered drug regulation by bypassing traditional clinical trial requirements, creating a template for accessing unapproved medicines that can be applied to other substances. This change affects how new treatments are controlled and how patient safety is upheld, as detailed in the introductory section of this article.
Q: How has the Special Access Scheme (SAS) changed for medicinal cannabis?
A: Originally intended as a narrow channel for very rare situations, the SAS has undergone a significant transformation, becoming the primary pathway for medicinal cannabis. With approvals increasing substantially, it has transformed into a mass-market distribution system for unapproved products, straining administrative resources and shifting its function from an exception to a default pathway for market entry.
Q: What are the key regulatory differences for medicinal cannabis compared to traditional drugs?
A: Medicinal cannabis products accessed via SAS largely circumvent traditional evidence thresholds, meaning they haven't undergone the full TGA evaluation for safety, quality, or efficacy. The approval process is inverted, granting market access first, and significant medico-legal liability is shifted to individual prescribers rather than regulatory bodies or manufacturers. This effectively created a 'Refusal Loophole' for market entry.
Q: How does the psychedelics advocacy model mirror the medicinal cannabis approach?
A: Advocates for therapeutic psychedelics have adopted a similar strategy to cannabis, utilizing individual SAS-B approvals to advance clinical practice ahead of traditional drug registration evidence. This model places liability on practitioners and relies on preliminary research and patient advocacy for market access, operating on assumptions regarding evidence and risk akin to the medicinal cannabis pathway.
Q: What challenges does the de facto market for unapproved medicines present?
A: This unofficial market lacks quality standardization, leading to variable product composition and purity. It also features inconsistent prescribing practices among doctors, fragmented safety monitoring systems with typically low reporting rates for adverse effects, and complex supply chains that increase the risks of product misuse, counterfeiting, and poor storage conditions, often creating a 'Retail Bottleneck' in patient access.
Q: What are the "regulatory costs" associated with the medicinal cannabis program?
A: The program imposes substantial, often overlooked, administrative costs on the Australian government for processing applications and monitoring compliance. There are also increased enforcement costs for bodies like the Office of Drug Control (ODC), and significant public health monitoring expenses due to the absence of robust pre-market clinical trials. These costs are a direct consequence of managing a large-scale unapproved medicines program.
Q: How does Chronic Care Pharmacy address these regulatory complexities?
A: Chronic Care Pharmacy employs a PhD-led Clinical Command Centre for real-time clinical safety validation, secure Schedule 8 handling with biometric controls, and seamless API integration for high-throughput processing. They utilize comprehensive traceability systems and offer doctorate-level risk analysis to ensure patient safety and help reduce prescriber liability within this complex regulatory environment.
Q: What are the TGA's compliance priorities for 2026-27 regarding medicinal cannabis?
A: The TGA has indicated increased scrutiny of medicinal cannabis operations as a compliance priority for 2026-27, signaling a proactive, risk-based approach to enforcement. This aims to impose more structure on the de facto market created by the SAS pathway. Recent submissions from the Australian Medical Association (AMA) and TGA consultations in late 2025 further underscore efforts to enhance oversight and address safety concerns regarding unapproved medicinal cannabis products.
Citations
- [1] https://www.tga.gov.au/resources/explore-topic/medicinal-cannabis-hub/medicinal-cannabis-guidance-documents/guidance-use-medicinal-cannabis-treatment-palliative-care-patients-australia
- [2] https://www.tga.gov.au/resources/explore-topic/medicinal-cannabis-hub/medicinal-cannabis-guidance-documents/guidance-use-medicinal-cannabis-australia-patient-information
- [3] https://www.odc.gov.au/medicinal-cannabis
- [4] https://www1.racgp.org.au/newsgp/professional/tga-reveals-compliance-priorities
- [5] https://www.tga.gov.au/news/media-releases/tga-releases-compliance-principles-reinforcing-proactive-and-risk-based-enforcement-throughout-2026-and-2027
- [6] https://www.tga.gov.au/news/news-articles/therapeutic-goods-legislation-amendment-effective-1-october-2025
- [7] https://www.tga.gov.au/resources/explore-topic/medicinal-cannabis-hub
- [8] https://www.abc.net.au/news/2025-10-27/act-two-years-on-from-drug-decriminalisation-laws/105938834
- [9] https://www.act.gov.au/health/drugs-alcohol-smoking-and-vaping/drug-law-reform
- [10] https://www.ojp.gov/ncjrs/virtual-library/abstracts/politics-implementing-drug-law-reform-australia
- [11] https://www.cannabiz.com.au/sas-b-deep-dive-approvals-climb-26-in-2025-as-flower-overtakes-oil-and-pastilles-surge
- [12] https://businessofcannabis.com/inside-australias-medical-cannabis-boom-prescriptions-products-patients
- [13] https://www.imarcgroup.com/australia-medical-cannabis-market
- [14] https://www.ama.com.au/articles/ama-submission-tga-review-safety-and-regulatory-oversight-unapproved-medicinal-cannabis
- [15] https://www.tga.gov.au/news/news/planned-consultation-address-growing-safety-concerns-unapproved-medicinal-cannabis-products-australia
- [16] https://www.odc.gov.au/sites/default/files/2025-06/cost-recovery-implementation-statement-regulation-of-medicinal-cannabis-2025-26.pdf
- [17] https://www.mcw.com.au/tga-advertising-and-medical-cannabis-enforcement-activity-top-10-trends
- [18] https://avant.org.au/resources/prescribing-medicinal-cannabis-be-aware-of-the-medico-legal-risks
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Discover how medicinal cannabis in Australia has shifted from stigma to acceptance, with insights on professional gaps and specialized infrastructure like Chronic Care Pharmacy for safe chronic care.
.jpg)
Explore the GP's dilemma in prescribing medicinal cannabis in Australia: navigate knowledge gaps, regulatory barriers, and solutions for confident, safe practice.
.jpg)
Discover how telehealth clinics and TGA reforms are transforming medicinal cannabis access in Australia, bridging rural gaps with efficient, compliant pharmacy fulfillment.
%20(1).svg)
