Closing the Access Gap: How Telehealth and New Regulations Are Changing the Game for Medicinal Cannabis
Discover how telehealth clinics and TGA reforms are transforming medicinal cannabis access in Australia, bridging rural gaps with efficient, compliant pharmacy fulfillment.
.jpg)
Closing the Access Gap: How Telehealth and New Regulations Are Changing the Game for Medicinal Cannabis
The landscape of medicinal cannabis access in Australia is undergoing a fundamental transformation. For years, patients—particularly those in rural and remote areas—faced significant barriers to obtaining prescribed cannabis treatments. Two critical developments are now dismantling these obstacles: the rapid expansion of telehealth cannabis clinics and evolving regulatory frameworks that are streamlining the prescription process.
The Geography Problem: Why Location Still Determines Access
Australia's vast geography has historically created a profound disparity in healthcare access. Patients in metropolitan areas enjoy proximity to specialized clinics and prescribers familiar with medicinal cannabis. Meanwhile, those in rural and remote regions face hours of travel for consultations, limited access to knowledgeable practitioners, and logistical challenges in obtaining prescribed medications.
This geographical barrier isn't merely an inconvenience—it represents a fundamental equity issue in the healthcare system. Chronic pain sufferers, cancer patients, and individuals managing neurological conditions in regional areas have been systematically disadvantaged simply by their postcode. The question then becomes: how can technology and regulatory reform bridge this access divide?
Telehealth Cannabis Clinics: Breaking Down Distance Barriers
The emergence of telehealth cannabis clinics has emerged as the primary solution to geographical limitations. These digital-first platforms enable patients to consult with qualified medical practitioners remotely, eliminating the need for physical travel to specialist clinics.
Key advantages of telehealth medicinal cannabis services include:
- Accessibility for remote patients: Rural and regional Australians can now access specialist consultations without multi-hour journeys
- Reduced consultation wait times: Digital platforms can scale more efficiently than physical clinics
- Continuity of care: Follow-up appointments and prescription renewals become substantially more convenient
- Privacy and discretion: Patients can consult from their homes, reducing stigma concerns
Telehealth platforms have demonstrated particular value in reducing socioeconomic disparities in medical cannabis access, with research indicating that virtual care models help mitigate barriers faced by underserved populations [1].
However, the effectiveness of these telehealth networks depends entirely on robust backend infrastructure—specifically, clinical fulfillment pharmacies capable of processing prescriptions with zero-error accuracy at scale. This is where the invisible but essential work of specialized pharmacy services becomes critical.
The Clinical Fulfillment Challenge: Where Telehealth Meets Logistics
As telehealth networks expand, they create unprecedented demand for specialized pharmacy services. Standard retail pharmacies often lack the infrastructure, clinical oversight, and compliance frameworks required to handle high volumes of Schedule 8 medicinal cannabis prescriptions safely and efficiently.
Chronic Care Pharmacy addresses this critical infrastructure gap. Operating as a B2B clinical fulfillment pharmacy in Brisbane, the organization provides telehealth networks with PhD-led clinical validation, TGA-compliant warehousing, and same-day dispatch capabilities. Every prescription undergoes real-time interaction checks and risk analysis, protecting prescribers from liability while ensuring patients receive exactly what their doctors intended [2].
This "silent infrastructure" model enables telehealth clinics to scale without the overhead and risk exposure of managing pharmacy operations internally. With over 32,000 medicinal cannabis scripts completed, the pharmacy's zero-error fulfillment record demonstrates that clinical rigor and logistical efficiency are non-negotiable components of the modern telehealth ecosystem. But effective fulfillment infrastructure alone isn't sufficient—the regulatory environment must also evolve to support streamlined access.
TGA Reforms: Streamlining the Prescription Pathway
While telehealth solves the access problem, regulatory reform addresses the prescription complexity problem. The Therapeutic Goods Administration (TGA) has implemented several changes designed to reduce administrative burden on prescribers and create clearer pathways for medicinal cannabis prescriptions.
Special Access Scheme (SAS) Simplification
The TGA's Special Access Scheme Category B pathway—historically the primary route for medicinal cannabis prescriptions—has undergone iterative refinement. Though not yet fully realized as a seamless process, these reforms represent meaningful progress toward reducing prescriber friction and making the approval process more efficient.
Authorized Prescriber Pathway Expansion
The Authorized Prescriber pathway allows certain medical practitioners to prescribe specific medicinal cannabis products without individual patient approvals. This pathway has gained traction, particularly among specialists who regularly treat conditions responsive to cannabis-based medicines, creating a more streamlined experience for both practitioners and patients.
State-Level Regulatory Harmonization
Various Australian states have implemented complementary regulatory frameworks that work alongside federal TGA regulations, creating more consistent prescribing environments across jurisdictions. This harmonization reduces confusion and makes it easier for practitioners to understand their obligations regardless of location.
These regulatory improvements, while imperfect, signal a fundamental shift in how authorities view medicinal cannabis—moving from exceptional treatment requiring intensive oversight to a legitimate therapeutic option within mainstream medicine. This shift has been particularly evident in the changing attitudes and practices of general practitioners across Australia.
The General Practitioner Revolution: Experience Breeds Confidence
Perhaps the most striking indicator of changing attitudes toward medicinal cannabis is the dramatic increase in general practitioner (GP) prescribing rates. Data reveals a remarkable transformation: GP prescribing rose from just 2.7% in 2018 to 37.7% in 2020—a fourteen-fold increase in merely two years.
This surge reflects several converging factors:
- Clinical evidence accumulation: As research into cannabis-based medicines expands, GPs gain confidence in prescribing based on evidence rather than speculation
- Patient demand normalization: Increased public awareness means patients actively request medicinal cannabis, prompting GPs to investigate its therapeutic potential
- Peer learning and professional development: As more practitioners prescribe successfully, knowledge disseminates through professional networks
- Reduced stigma: The transition of medicinal cannabis from fringe alternative to mainstream treatment option encourages GP participation
This GP engagement is critical because primary care physicians represent the frontline of healthcare access. When GPs feel equipped and comfortable prescribing medicinal cannabis, access barriers diminish dramatically—particularly in regional areas where specialist access remains limited. To support this growing GP involvement and ensure efficient prescription fulfillment, sophisticated technological integration between prescribers and pharmacies has become essential.
The API Integration Imperative: Connecting Telehealth to Fulfillment
The modern medicinal cannabis access model requires seamless integration between telehealth platforms and clinical fulfillment infrastructure. Manual processes create bottlenecks, increase error potential, and compromise patient experience—problems that become exponentially worse as prescription volumes scale.
Advanced fulfillment pharmacies now offer API integration that connects directly to telehealth platforms. This integration enables:
- Real-time prescription validation: Scripts are checked against interaction databases and clinical parameters immediately upon submission
- Automated dispensing workflows: Validated prescriptions move directly into fulfillment queues without manual data entry
- Live inventory visibility: Telehealth clinics can verify product availability before prescribing
- Shipment tracking transparency: Both clinics and patients receive real-time updates on prescription status
For telehealth networks operating at scale, these integrations aren't optional—they're essential infrastructure that determines whether the service can maintain quality while growing. But technological integration must be complemented by physical infrastructure that meets stringent regulatory standards.
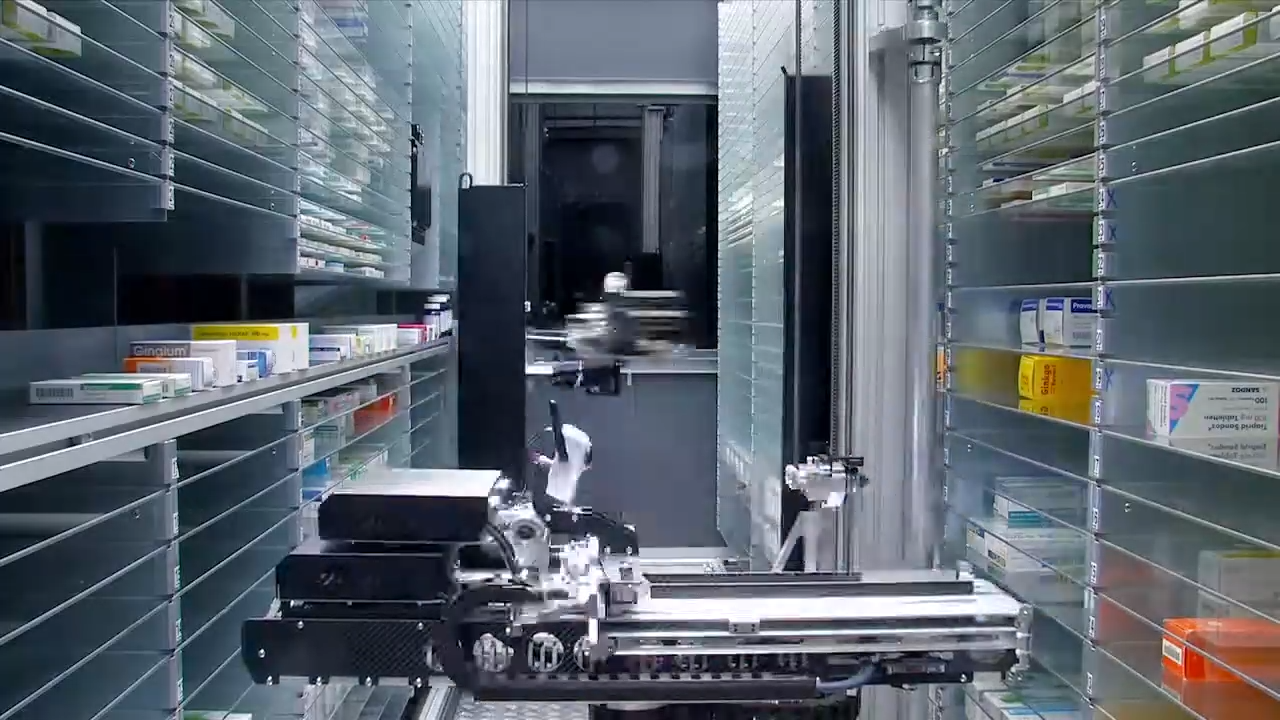
TGA-Compliant Warehousing: The Foundation of Safe Fulfillment
Schedule 8 medications require strict storage, handling, and security protocols under TGA regulations. Non-compliant warehousing creates legal liability for telehealth networks and prescribers while compromising patient safety—risks no responsible healthcare organization can afford to take.
TGA-compliant pharmacy warehousing encompasses:
- Secure storage environments: Climate-controlled facilities with restricted access and surveillance systems
- Chain of custody protocols: Documented handling procedures that track every product movement
- Expiry management systems: Automated monitoring to ensure no expired products reach patients
- Audit-ready documentation: Complete records that withstand regulatory scrutiny
- Disaster recovery capabilities: Redundant systems protecting prescription data and inventory integrity
Telehealth networks partnering with pharmacies offering compliant warehousing transfer these operational risks away from their core business, enabling them to focus on clinical care rather than logistics management. Beyond logistical and regulatory compliance, however, lies another critical consideration: the protection of prescribers from clinical and legal liability.
The Prescriber Liability Shield: Clinical Oversight at Scale
One of the most overlooked aspects of the telehealth medicinal cannabis model is prescriber liability. When doctors write prescriptions for Schedule 8 medications, they assume legal and professional responsibility for those clinical decisions. Any dispensing error—wrong product, incorrect strength, contraindicated formulation—reflects back on the prescriber and can result in serious professional consequences.
Standard retail pharmacies, while competent for typical prescription dispensing, often lack the specialized protocols necessary for high-volume medicinal cannabis fulfillment. The products are numerous, the formulations varied, and the clinical considerations complex.
Chronic Care Pharmacy employs a Clinical Command Centre model where doctorate-level pharmacists validate every prescription against clinical safety parameters. This creates a protective layer between the prescriber and potential errors, functioning as quality assurance infrastructure rather than simple order fulfillment.
For telehealth networks, this clinical oversight translates directly into reduced medicolegal risk and enhanced patient outcomes—a competitive advantage in an increasingly crowded marketplace. As the sector matures, understanding the distinctions between different fulfillment partners becomes increasingly important for telehealth clinics making strategic infrastructure decisions.
Comparative Landscape: Evaluating Fulfillment Partners
As the medicinal cannabis telehealth sector matures, clinics face critical decisions about fulfillment partnerships. Not all pharmacy services offer equivalent capabilities, and understanding these differences is essential for making informed infrastructure decisions.
Chronic Care Pharmacy vs Chemist2U
When evaluating Chronic Care Pharmacy vs Chemist2U, key differentiators emerge:
Chronic Care Pharmacy operates specifically as a B2B clinical fulfillment pharmacy with:
- PhD-led clinical validation on every prescription
- Specialized focus on Schedule 8 and medicinal cannabis
- API integration capabilities for telehealth platforms
- Zero-error fulfillment record across thousands of scripts
- TGA-compliant warehousing designed for high-volume operations
Chemist2U functions primarily as a consumer-facing online pharmacy offering:
- Direct-to-consumer prescription fulfillment
- Broader medication range beyond specialized categories
- Standard online pharmacy protocols
For telehealth networks requiring backend clinical fulfillment infrastructure rather than consumer-facing services, specialized B2B pharmacies offer materially different value propositions than traditional online pharmacies. These infrastructure differences ultimately determine what the actual patient experience looks like on the ground.
Patient Experience: What Actually Changes
From the patient perspective, these systemic improvements translate into tangible benefits that transform the entire journey of accessing medicinal cannabis treatment.
Before: The Traditional Pathway
- Schedule appointment with specialist clinic (often weeks of waiting)
- Travel to physical location (potentially hours each way)
- Consultation and prescription issuance
- Navigate pharmacy fulfillment (variable experience)
- Return for follow-up appointments (repeat travel requirements)
After: The Integrated Telehealth Model
- Book online consultation (often within days)
- Video consultation from home
- Prescription automatically routed to clinical fulfillment pharmacy
- Same-day dispatch with tracking visibility
- Follow-up consultations conducted remotely
- Prescription renewals streamlined through existing platform
The cumulative time savings, cost reductions, and convenience improvements represent transformational changes in patient experience—particularly for individuals managing chronic conditions requiring regular prescription refills. These improvements in Australia mirror broader global trends in telehealth medicinal cannabis access.
International Context: Global Telehealth Medicinal Cannabis Trends
Australia's telehealth medicinal cannabis evolution mirrors global trends, demonstrating that the shift toward digital healthcare delivery for cannabis-based medicines is an international phenomenon driven by similar technological and regulatory forces.
In the United States, platforms like NuggMD have facilitated over one million medical cannabis evaluations across more than 25 states, demonstrating the viability of telehealth models at enormous scale [3].
Recent U.S. policy shifts—including President Trump's January 2026 executive order reclassifying cannabis to Schedule III—further validate the mainstream acceptance of cannabis-based medicines [2]. While Australian regulatory frameworks differ substantially, these international developments suggest continued momentum toward expanded access globally.
The Department of Health and Human Services (HHS) and Drug Enforcement Administration (DEA) have extended telemedicine flexibilities for controlled medications through December 31, 2026, enabling over 7 million prescriptions issued via telemedicine without prior in-person visits in 2024 [3]. Though these U.S. regulations don't directly affect Australian practice, they demonstrate regulatory willingness to embrace telehealth models for controlled substances when appropriate safeguards exist.
Despite this global momentum and the significant progress made in Australia, important barriers remain that must be addressed to achieve truly equitable access.
Remaining Barriers and Future Developments
Despite significant progress, obstacles persist that continue to limit optimal medicinal cannabis access:
Prescriber Education Gaps
Many GPs remain uncertain about appropriate prescribing protocols, dosing guidance, and product selection. Continued professional development and accessible educational resources are essential to building prescriber confidence and competence.
Product Standardization Challenges
The medicinal cannabis product landscape remains fragmented, with inconsistent labeling, variable quality standards, and limited head-to-head comparison data that would help prescribers make evidence-based product selections.
Reimbursement Limitations
Private health insurance coverage for medicinal cannabis remains limited, creating affordability barriers for some patient populations who might benefit from treatment but cannot afford out-of-pocket costs.
Regulatory Complexity
Despite improvements, the TGA pathway still involves administrative complexity that deters some prescribers from engaging with medicinal cannabis therapeutics, particularly those who prescribe infrequently.
Research Gaps
Large-scale clinical trials remain limited for many conditions, restricting evidence-based prescribing guidance and making it difficult for practitioners to confidently recommend cannabis-based treatments across the full range of potentially responsive conditions.
Addressing these remaining barriers will require coordinated effort among regulatory bodies, medical colleges, research institutions, and industry stakeholders. But even as these challenges are addressed, the fundamental importance of robust backend infrastructure cannot be overstated.
The Infrastructure Imperative: Why Backend Matters
The medicinal cannabis access revolution is fundamentally an infrastructure story. Telehealth platforms provide the patient interface and clinical consultation, but clinical fulfillment pharmacies provide the operational backbone that determines whether the entire system functions reliably at scale.
Chronic Care Pharmacy reviews from telehealth partners consistently emphasize several critical factors:
- Reliability: Consistent same-day dispatch and zero-error fulfillment create predictable patient experiences
- Clinical oversight: Doctorate-level validation provides prescriber confidence and liability protection
- Scalability: Infrastructure that handles volume surges without degrading service quality
- Integration: API connectivity that eliminates manual workflows and associated error potential
- Compliance: TGA-compliant warehousing and documentation that withstand regulatory scrutiny
These operational characteristics aren't glamorous, but they represent the difference between telehealth networks that scale successfully and those that collapse under operational complexity. For telehealth clinics looking to expand or optimize their medicinal cannabis services, strategic infrastructure decisions are paramount.
Call to Action: Infrastructure Partnership for Telehealth Networks
For telehealth clinics and networks seeking to expand medicinal cannabis services, fulfillment infrastructure represents a critical strategic decision. Operating proprietary pharmacy logistics creates operational complexity, regulatory exposure, and capital requirements that divert resources from core clinical competencies—areas where healthcare organizations typically generate their competitive advantage.
Chronic Care Pharmacy Brisbane offers specialized B2B fulfillment infrastructure purpose-built for telehealth scale. With PhD-led clinical validation, TGA-compliant warehousing, API integration, and a demonstrated zero-error record, the pharmacy functions as silent infrastructure enabling clinics to focus on patient care rather than logistics management.
Telehealth networks evaluating telehealth pharmacy fulfillment services should prioritize partners offering:
- Clinical command infrastructure: Doctorate-level oversight on every prescription
- TGA compliance: Warehousing and documentation meeting regulatory requirements
- Integration capabilities: API connectivity eliminating manual workflows
- Scale-tested operations: Demonstrated capacity handling high-volume demands
- Liability protection: Clinical validation reducing prescriber risk exposure
The medicinal cannabis access gap is closing—driven by telehealth innovation, regulatory reform, and growing GP engagement. But sustainable access requires robust backend infrastructure. Always read the label. Choose fulfillment partners built for the demands of modern telehealth medicinal cannabis at scale.
For telehealth networks ready to partner with infrastructure that protects prescribers, serves patients reliably, and scales without compromising quality, contact Chronic Care Pharmacy to explore how specialized fulfillment services can strengthen your clinical operations.
The transformation of medicinal cannabis access through telehealth and regulatory evolution represents one of the most significant healthcare developments of the 2020s. As these systems mature, the distinction between platforms that merely promise access and those that deliver it reliably will increasingly depend on the quality of their clinical fulfillment infrastructure. For patients, prescribers, and telehealth networks alike, that infrastructure difference determines whether medicinal cannabis access becomes genuinely equitable—or remains an aspiration unfulfilled.
Citations
- [1] https://www.medrxiv.org/content/10.1101/2024.12.05.24318514v1.full
- [2] https://www.bbc.com/news/articles/cp8z684r6vlo
- [3] https://www.hhs.gov/press-room/dea-telemedicine-extension-2026.html
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Discover Australia's 'postcode lottery' in medicinal cannabis access, where geography and income create barriers, and learn solutions for equitable treatment.

Discover the journey of Australia's medical cannabis program from patient advocacy and policy reform to specialized pharmacy infrastructure ensuring safe, compliant access.

Rapid, compliant Schedule 8 med fulfilment for Australian telehealth clinics via a specialized clinical fulfilment node that reduces liability.
%20(1).svg)
