From Patient Advocacy to Policy: The Story Behind Australia's Medical Cannabis Program
Discover the journey of Australia's medical cannabis program from patient advocacy and policy reform to specialized pharmacy infrastructure ensuring safe, compliant access.

From Patient Advocacy to Policy: The Story Behind Australia's Medical Cannabis Program
Australia's medical cannabis program stands as a testament to the power of patient advocacy, strategic philanthropy, and evidence-based policy reform. Born from personal tragedy and sustained by coordinated efforts across multiple sectors, the program has evolved from a grassroots movement into a comprehensive regulatory framework. This article examines the journey from advocacy to implementation, exploring how Australia's prescription-based model emerged and why specialized pharmacy infrastructure has become critical to its success.
Since the landmark 2016 federal legislation, the effective prescription, dispensing, and fulfillment of Schedule 8 medicinal cannabis medications have become paramount to ensuring patient access while maintaining clinical safety. At Chronic Care Pharmacy, we are Australia's leading specialized pharmacy partner, ensuring compliant and rapid access to medicinal cannabis, cutting through complexity for clinics and patients alike. We empower clinics and prescribers by transforming complex regulatory challenges into seamless patient care, bridging the gap between Australia's medicinal cannabis regulations and guaranteed patient access.
The Advocacy Foundation: United in Compassion and Parent-Led Campaigns
The path to legislative reform began not in parliamentary chambers, but in family homes across Australia. The main driver for Australia's medicinal cannabis program was a well-organized advocacy campaign led by parents who had witnessed significant health benefits when treating their children with illegal cannabis products [1]. Despite facing legal risks, these families documented compelling improvements for conditions ranging from childhood epilepsy to chemotherapy-induced nausea, where traditional medicines had failed.
The Haslam Family's Pivotal Role
Central to this movement was the story of Dan Haslam and his family. Diagnosed with terminal bowel cancer at age 20, Dan suffered severe side effects from chemotherapy and opiate painkillers that left him unable to function [2]. His parents, Lou (a former police officer) and Lucy (a retired nurse), made the difficult decision to provide him with cannabis tincture, even though it was against the law.
Dan experienced immediate, documented relief. He regained his appetite, reduced his reliance on pharmaceutical opiates, and achieved a quality of life impossible with conventional pain management methods [3]. This personal experience transformed Lucy Haslam into one of Australia's most prominent advocates for medicinal cannabis and catalyzed a national conversation about compassionate access to alternative treatments.
In 2014, Lucy Haslam co-founded United in Compassion (UIC), which quickly became Australia's leading medicinal cannabis advocacy group [1]. The organization focused on:
- Advocating for patients to access full-spectrum herbal medicinal cannabis extracts
- Promoting education based on evidence about the clinical uses of cannabis
- Campaigning for changes to regulations to improve patient access
- Highlighting systemic failures in managing chronic illnesses
Dan Haslam's death on February 24, 2015, at age 25, occurred as political momentum was building [4]. His story profoundly influenced then-NSW Premier Mike Baird's view, leading to commitments for clinical trials for terminally ill patients. The Haslam family pledged to continue Dan's advocacy, ensuring his legacy would drive the legislative change he never lived to see.
Strategic Philanthropy: The Lambert Initiative
While advocacy created essential political pressure and public awareness, institutional research infrastructure provided the clinical evidence needed for regulatory reform. In 2015, a $34 million donation to the University of Sydney established the Lambert Initiative for Cannabinoid Therapeutics—one of the largest philanthropic gifts in Australian medical research history.
This substantial funding created a dedicated research center focused on:
- Clinical trials studying how well cannabinoids work for various conditions
- Pharmacological analysis of different cannabis formulas
- Safety and dosing guidelines for medical practitioners
- Summarizing research findings to help inform regulatory decisions
The Lambert Initiative filled a critical gap: the lack of local clinical data to guide prescribing, inform Therapeutic Goods Administration (TGA) approvals, and set safety standards for Schedule 8 medication dispensing. This research infrastructure signaled to policymakers that medicinal cannabis could be integrated into existing pharmaceutical regulatory frameworks, rather than requiring entirely new oversight mechanisms. The combination of patient advocacy and rigorous scientific research created the foundation for meaningful policy change.
The Victorian Blueprint: Law Reform Commission's 2015 Report
Victoria provided the most comprehensive roadmap for legislative implementation. The Victorian Law Reform Commission's 2015 report offered a detailed blueprint that synthesized international models, Australian legal frameworks, and clinical safety information into actionable policy recommendations.
Key Recommendations
The Commission's report addressed fundamental questions about program implementation:
- Regulatory Classification: How should medicinal cannabis be categorized within existing poison controls?
- Prescribing Authority: Which medical practitioners should be allowed to prescribe, and under what conditions?
- Supply Chain Controls: What manufacturing, distribution, and dispensing rules are needed to ensure product quality and prevent diversion?
- Patient Access Pathways: How should approval processes balance patient accessibility with clinical oversight?
The report's evidence-based approach and detailed regulatory structure provided the framework that would inform federal action. It demonstrated that legalizing medicinal cannabis could apply proven regulatory models to a new therapeutic category without compromising existing safety measures. This careful balancing act between access and control would become a defining characteristic of Australia's approach.
Federal Legislation: The 2016 Framework
On February 24, 2016—the one-year anniversary of Dan Haslam's death—the federal Parliament amended the Narcotic Drugs Act 1967, creating a legal pathway for cultivating, manufacturing, and clinically using medicinal cannabis. This legislation, often called "Dan's Law" in recognition of the advocacy that made it possible, established:
- A licensing system for domestic cultivation and production
- Therapeutic Goods Administration (TGA) oversight for product quality and safety standards
- Prescribing pathways through the Special Access Scheme (SAS) and Authorized Prescriber programs
- Requirements for state and territory cooperation during implementation
The legal framework integrated medicinal cannabis within Australia's existing prescription medicine system, rather than creating a separate regulatory structure. This decision had profound implications for pharmacy operations, particularly those specializing in Schedule 8 medication dispensing and telehealth pharmacy fulfillment services.
For organizations like Chronic Care Pharmacy in Brisbane, the prescription-based model meant that fulfilling medicinal cannabis prescriptions required the same strict safety protocols, real-time clinical validation, and risk analysis frameworks applied to other controlled substances. This approach distinguished Australia's system from international alternatives while creating both opportunities and challenges for implementation.
Comparative International Models
Understanding Australia's unique approach requires examining how other countries have addressed medicinal cannabis regulation. Australia's prescription-based regulatory framework contrasts significantly with medicinal cannabis programs in other jurisdictions:
CountryModelKey FeaturesUnited StatesState-Level Medical ProgramsFragmented state-by-state model with no federal framework. Each state sets its own qualifying conditions, dispensary licensing, patient registration, and product testing standards. This creates inconsistencies and limits national pharmacy network integration.CanadaHybrid Prescription & Licensed Producer SystemInitially prescription-based (2001-2018), then adult-use legalized. Doctors authorized patients, and licensed producers shipped directly. Traditional pharmacy dispensing was largely excluded, creating separate fulfillment pathways.IsraelHospital-Centric Specialized DistributionOne of the oldest programs (1990s). Operates through specialized cannabis units within hospitals. Centralized supply from licensed government contractors, doctor authorization with continuous monitoring. Limited community pharmacy involvement.NetherlandsPharmacy Dispensing ModelPioneered pharmacy-based distribution. Government's Office of Medicinal Cannabis supplies standardized products to pharmacies. Pharmaceutical-grade cannabis available with prescriptions, integrated with existing pharmacy operations, and standardized quality control. Insurance coverage in specific situations.
Australia's model shares structural similarities with the Netherlands' approach, particularly concerning pharmacy integration and Therapeutic Goods Administration (TGA)-compliant quality standards. However, Australia's regulatory framework extends more broadly to encompass licensed cultivation, diverse product formats, and telehealth authorization pathways. Unlike traditional dispensaries, specialized clinical fulfillment pharmacies like Chronic Care Pharmacy are deeply embedded in this regulated, prescription-driven framework, serving as critical infrastructure for program success.
Implementation Challenges and Sector Evolution
While the 2016 legislation created legal pathways, translating policy into practice revealed significant operational challenges that continue to shape the sector's evolution.
Access Barriers
Despite legalization, patient access remained constrained by multiple factors:
- Complex authorization processes requiring specialist knowledge and navigation skills
- Limited awareness and training among general practitioners and specialists
- High out-of-pocket costs without Pharmaceutical Benefits Scheme (PBS) subsidies
- Product availability limitations during the industry's early development stages
In a powerful reflection on the program's development, Lucy Haslam stated, "The medicinal cannabis law was named after my son. Now, shady companies are damaging his legacy" [5]. She expressed concern that current practices often prioritize profit over patient care, with some providers offering "unfettered access" without proper clinical assessment. This tension between accessibility and clinical rigor underscores the critical importance of pharmacy infrastructure that maintains therapeutic oversight while ensuring efficient fulfillment.
Clinical Safety Requirements
The Schedule 8 classification of most medicinal cannabis products imposes strict dispensing and record-keeping obligations on pharmacies. Medication dispensing errors represent a well-documented challenge in healthcare, with studies indicating average error rates around 4 per 100 prescriptions dispensed in general pharmacy settings [10]. These errors, which can range from incorrect dosages to product mismatches, constitute a frequent and avoidable source of patient harm, particularly with complex medications [11].
For Schedule 8 medicinal cannabis medications, the consequences of such errors—including the Refusal Loophole where non-compliant prescriptions are rejected—are compounded by the urgency of patient need and the strict regulatory environment. Essential requirements include:
- Real-time prescription validation against prescriber authority
- Complete audit trails for regulatory compliance
- Secure storage meeting controlled substance standards
- Monitoring and reporting protocols to prevent diversion
Regulatory bodies like the TGA and Ahpra increasingly scrutinize prescribing and dispensing practices, with significant fines and professional repercussions for non-compliance [9] [12]. For instance, a single company was recently fined $118,800 for advertising breaches related to medicinal cannabis [13], underscoring the financial risks of regulatory missteps.
Medicinal cannabis fulfillment pharmacies must implement systems that not only meet these regulatory demands but also actively prevent errors while maintaining rapid fulfillment for telehealth networks and multi-clinic partnerships. This proactive approach significantly reduces legal liability for clinical practices, ensuring compliance with complex Schedule 8 regulations.
Quality Assurance and Product Standardization
Unlike well-established pharmaceutical products, medicinal cannabis products exhibit significant compositional variability:
- Ratios of tetrahydrocannabinol (THC) and cannabidiol (CBD), and other cannabinoids
- Terpene profiles that influence therapeutic effects
- Bioavailability differences across formats (oils, dried flower, capsules)
- Batch-to-batch consistency challenges
This complexity necessitates sophisticated inventory management systems that track product characteristics, expiry dates, and batch numbers—capabilities essential for Therapeutic Goods Administration (TGA)-compliant pharmacy warehousing. These technical requirements further emphasize why specialized pharmacy infrastructure has become indispensable to program success.
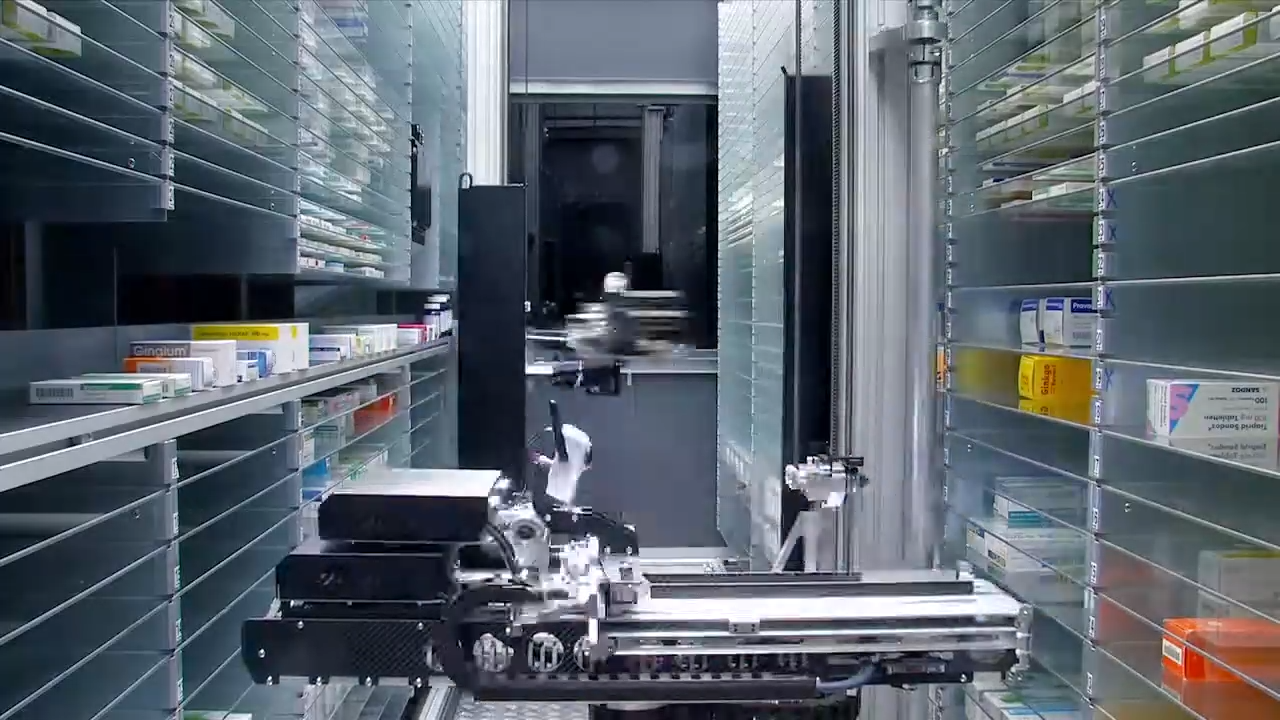
The Role of Specialized Pharmacy Infrastructure
The prescription-based framework positions pharmacies as critical control points within Australia's medicinal cannabis ecosystem. Effective system operation requires pharmacy infrastructure that integrates multiple complex functions:
- Clinical validation: Verifying prescriber authorization and patient eligibility before dispensing
- Regulatory compliance: Maintaining comprehensive records meeting state and federal requirements
- Logistics efficiency: Ensuring same-day or next-day dispatch to support continuous treatment
- Risk mitigation: Implementing safety protocols that protect clinical practices from legal liability
Chronic Care Pharmacy in Brisbane exemplifies this specialized infrastructure. Rather than operating as a traditional dispensary, we function as a PhD-led Clinical Command Centre designed to enforce a near 'zero-error' standard. Our system validates every Schedule 8 prescription through real-time clinical safety analysis, forming a robust RTPM ecosystem that minimizes dispensing error risk and ensures immediate compliance.
Our clinical fulfillment services deliver:
- Peace of mind: With over 32,000 medicinal cannabis scripts successfully completed, our expertise is proven
- Rapid patient access: Our fulfillment velocity averages under 4 hours, ensuring timely medication delivery
- Minimized practice liability: Experience a 2X reduction in legal risk for our clinical partners through our robust Clinical Safety Net
Such specialized operations demonstrate how dedicated pharmacy logistics can support telehealth networks while maintaining the clinical rigor intended by Australia's legislative framework. To learn more about our comprehensive clinical fulfillment services and how we partner with clinics across Australia, visit our services page.
Current State: Advocacy Continues
As of January 2026, over one million Australians have been legally authorized to use medicinal cannabis [9] [6]. This remarkable growth demonstrates the program's success in providing legal access where none existed before. Yet, significant challenges persist that continue to mobilize advocacy efforts:
- Cost barriers: Out-of-pocket expenses remain prohibitively high for many patients
- Prescriber education gaps: Many healthcare professionals lack adequate training on cannabinoid therapeutics and the endocannabinoid system
- Persistent stigma: Social and professional attitudes continue to influence prescribing decisions and patient disclosure
- Quality variability: Ongoing concerns about unethical online clinic practices and inadequate patient care
Advocacy organizations, including United in Compassion and the newly merged Australian Medicinal Cannabis Association (AMCA), continue campaigns focused on [7]:
- Improving patient access and affordability through regulatory reforms
- Changing employment and driving laws that unfairly penalize medicinal cannabis patients
- Promoting evidence-based education for prescribers
- Establishing quality standards across the entire clinical pathway
Recent surveys indicate strong public support for further integration: 64% of Australians support including medicinal cannabis into mainstream healthcare, with 75% agreeing it improves overall access [8]. This sustained public support suggests the advocacy movement that began with families like the Haslams continues to resonate broadly across Australian society.
Conclusion: From Advocacy to Infrastructure
Australia's medicinal cannabis program emerged from the convergence of personal tragedy, strategic advocacy, institutional research, and evidence-based policy reform. What began with families courageously sharing their stories and breaking the law to help their loved ones has evolved into a comprehensive regulatory framework serving over one million Australians.
The legislative framework established in 2016 created a prescription-based system that integrates medicinal cannabis into existing pharmaceutical regulatory structures—an approach that prioritizes clinical safety while enabling patient access. This distinctive Australian model, influenced by the evidence-based approach pioneered in the Victorian Law Reform Commission's report, represents a middle path between unregulated access and overly restrictive controls.
However, the program's ongoing success fundamentally relies on specialized pharmacy infrastructure capable of managing Schedule 8 medication dispensing at scale while upholding the strict clinical standards and regulatory compliance intended by the program's creators. For telehealth networks, multi-clinic operators, and prescribers navigating this complex landscape, partnering with dedicated medicinal cannabis pharmacy fulfillment services has become essential to delivering on the promise of safe, accessible treatment.
Chronic Care Pharmacy in Brisbane offers the robust infrastructure and clinical expertise required to deliver safe, efficient, and compliant patient care. Our advanced Clinical Command Centre operates with a 'zero-error' philosophy, effectively mitigating the Refusal Loophole and ensuring seamless patient access through unparalleled real-time validation and compliance protocols.
Always read the label and consult with qualified healthcare professionals regarding medicinal cannabis treatment options. To discuss how Chronic Care Pharmacy can support your clinical operations and enhance patient care, contact us today!
Method & Data
This analysis draws upon a historical review of legislative milestones, reports from key advocacy groups such as United in Compassion, government publications from the TGA, academic research from institutions like the Lambert Initiative, and insights into international regulatory models. Primary sources include parliamentary records, advocacy organization publications, and peer-reviewed research on medicinal cannabis regulation and pharmacy practice.
Limitations
- Reliance on publicly available documents and reports may not fully capture nuanced political negotiations or operational challenges faced during implementation
- Quantitative data on prescription refusal rates or specific patient outcomes linked to pharmacy fulfillment efficiency remain limited in publicly accessible literature
- The rapidly evolving nature of the medicinal cannabis sector means some market dynamics may change swiftly, potentially dating specific observations
- Analysis focuses primarily on the national framework, with less granular detail on state-specific implementation variations that may significantly affect local access
Next Steps
Further empirical research is needed to quantify the direct impact of specialized pharmacy infrastructure on patient outcomes, measure the economic burden of the Refusal Loophole on the healthcare system, and evaluate the long-term cost-effectiveness of Australia's prescription-based model compared to alternative international approaches.
Frequently Asked Questions (FAQ)
What is the "Refusal Loophole" in Australia's medical cannabis program?
The Refusal Loophole refers to instances where medicinal cannabis prescriptions are rejected due to errors or non-compliance with regulatory requirements. Studies show that general medication dispensing errors occur in approximately 4 out of every 100 prescriptions, which can lead to significant patient harm and access delays [10]. This challenge also carries significant financial and legal risks for clinics and prescribers, as regulatory bodies actively scrutinize practices. Specialized pharmacy systems, like those at Chronic Care Pharmacy, aim to mitigate this issue through advanced verification processes and expertise in Jurisdictional Arbitrage, ensuring near 'zero-error' fulfillment.
How did Dan Haslam contribute to Australia's medicinal cannabis program?
Dan Haslam's personal battle with terminal cancer and the relief he found with cannabis tincture, despite its illegality, brought significant public and political attention to medicinal cannabis. His story and his family's tireless advocacy were pivotal in driving legislative reform, leading to the 2016 federal law often called "Dan's Law" in his honor. His death on the day Parliament began considering the legislation added profound urgency to the reform movement.
What is the role of specialized pharmacy infrastructure in the program?
Specialized pharmacy infrastructure is crucial for managing the complex requirements of Schedule 8 medicinal cannabis medications. It encompasses clinical validation, strict regulatory compliance, efficient logistics for rapid dispatch, and risk mitigation protocols to ensure patient safety and legal adherence. Unlike traditional dispensaries, specialized clinical fulfillment pharmacies like Chronic Care Pharmacy provide an integrated, high-compliance solution with a 'zero-error' philosophy, drastically reducing dispensing risks and protecting clinics from regulatory pitfalls.
What is the Lambert Initiative for Cannabinoid Therapeutics?
The Lambert Initiative for Cannabinoid Therapeutics is a research center at the University of Sydney, established through a historic $34 million donation. It focuses on conducting clinical trials, analyzing cannabis formulations, and developing evidence-based safety and dosing guidelines to support policymakers and prescribers in making informed decisions about medicinal cannabis use.
How does Australia's medical cannabis model compare to international approaches?
Australia uses a prescription-based model integrated into existing pharmaceutical regulatory structures, sharing similarities with the Netherlands' pharmacy-centered approach. This contrasts with the fragmented state-level models in the United States, Canada's direct-to-patient licensed producer system, and Israel's hospital-centric distribution. Australia's model uniquely combines pharmaceutical-grade standards, TGA oversight, and specialized pharmacy fulfillment. You can find a detailed comparison in the Comparative International Models section above.
What are the main ongoing challenges for Australia's medical cannabis program?
Despite significant progress, ongoing challenges include high out-of-pocket costs for patients without PBS subsidies, gaps in prescriber education about cannabinoid therapeutics, persistent social and professional stigma around cannabis use, and concerns about quality variability and unethical practices in some clinics. Advocacy groups continue working to address these issues, improve patient access, enhance affordability, and establish consistent quality standards across the clinical pathway.
Citations
- [1] https://rcvmhs.archive.royalcommission.vic.gov.au/United_In_Compassion.pdf
- [2] https://ausmca.org
- [3] https://internationalcbc.com/australian-survey-64-support-medicinal-cannabis-as-mainstream-healthcare
- [4] https://www.smh.com.au/national/the-medicinal-cannabis-law-was-named-after-my-son-now-shady-companies-are-damaging-his-legacy-20250729-p5minz.html
- [5] https://anmj.org.au/qa-with-medicinal-cannabis-advocate-lucy-haslam
- [6] https://www.bbc.com/news/world-australia-47796044
- [7] https://www.sbs.com.au/news/article/haslam-family-vows-to-continue-campaigning/4hu13y8qr
- [8] https://www.smh.com.au/national/nsw/dan-haslam-who-changed-mike-bairds-views-on-medicinal-cannabis-dies-of-cancer-20150225-13o6pk.html
- [9] https://www.racgp.org.au/gp-news/media-releases/2025-media-releases/october-2025/health-bodies-urge-crackdown-on-rogue-operators-as
- [10] https://www.ncbi.nlm.nih.gov/books/NBK519065
- [11] https://www.nationalacademies.org/read/11623/chapter/15
- [12] https://www.9news.com.au/health/medicinal-cannabis-advertising-dispensed-tga-fine-australia/93b00c25-cb4e-4adf-a311-40994b56be61
- [13] https://www.news.com.au/lifestyle/health/health-problems/major-crackdown-on-medicinal-cannabis-doctor-writes-17k-scripts/news-story/8f9b45986884d806ef5d4bedb4e59b5d
Links
Everything you need to scale your clinic, without the retail overhead.
Other article
.jpg)
Explore the GP's dilemma in prescribing medicinal cannabis in Australia: navigate knowledge gaps, regulatory barriers, and solutions for confident, safe practice.

Explore financial and legal barriers to medical cannabis access in Australia, from high out-of-pocket costs to strict drug-driving laws, and paths to reform.

Discover Australia's 'postcode lottery' in medicinal cannabis access, where geography and income create barriers, and learn solutions for equitable treatment.
%20(1).svg)
