The Price of Relief: Unpacking the Barriers to Medical Cannabis Access in Australia
Explore financial and legal barriers to medical cannabis access in Australia, from high out-of-pocket costs to strict drug-driving laws, and paths to reform.

The Price of Relief: Unpacking the Barriers to Medical Cannabis Access in Australia
Despite medicinal cannabis becoming legal in Australia in 2016, patients continue to face persistent and often insurmountable hurdles accessing this crucial treatment option. Two main barriers stand out starkly in January 2026: the crippling financial costs and draconian state drug-driving laws. These issues create an unacceptable paradox where legal access exists on paper, but in reality, tens of thousands of patients in desperate need of relief from chronic conditions struggle to obtain the medication they legitimately require.
The Financial Burden of Medicinal Cannabis Treatment
Out-of-Pocket Costs Create Access Inequality
The most significant barrier to accessing medicinal cannabis in Australia remains the substantial financial cost to patients. According to the Cannabis as Medicine Survey 2020 (CAMS-20), prescribed medicinal cannabis cost patients an average of AUD $79.20 weekly. While this data is from 2020, more recent analyses indicate that despite market growth and increasing patient numbers, significant out-of-pocket expenses persist. For instance, Australia's medicinal cannabis market is projected to exceed AUD$1 billion in sales by the end of 2025, firmly establishing it as a major global market, yet without widespread subsidization, this spending largely comes directly from patients' pockets [7], [11].
As Rebecca E Olson and colleagues critically observe in their study, patients often experience 'financial toxicity,' a burden so severe it not only impacts their well-being but also tragically limits their ability to access necessary medication [1]. This crippling financial strain primarily exists because medicinal cannabis products are not subsidized by the Pharmaceutical Benefits Scheme (PBS), forcing patients to pay the full retail price out of pocket.
The total cost typically includes several components:
- Initial consultations: These typically cost between $29 and $89, depending on the healthcare provider [2].
- Follow-up appointments: Required for ongoing prescription management.
- Product costs: Highly variable based on product type, strength, and dosage.
- Dispensing fees: Pharmacies charge these for handling Schedule 8 medications.
Price Variability Across Product Types
Understanding the pricing structure helps patients anticipate their financial commitment. Medicinal cannabis products show significant price differences depending on their form, cannabinoid content, and the required dose. Here's a look at current Australian market prices:
Dried Flower $10–$15 per gram - Typical monthly cost: $400–$600 for high-THC products; 30g (22–30% THC) approx. $430 [3]
Oils & Tinctures $100–$300 per bottle - Cost per mg: $0.08 (balanced extracts), $0.04 (single-compound oils) [4]
Monthly Expenditure (Average) $100–$600 per month
Low-dose CBD therapy: $100–$200;
Moderate combination therapy: $200–$400;
High-THC treatment protocols: $400–$600 [5]
The average daily cost for medicinal cannabis treatment is around $9–$10, with monthly averages reaching $278 for typical treatment plans [4]. For many patients managing chronic conditions on fixed incomes, these costs represent a substantial portion of their household budget.
Systemic Factors Driving High Costs
Several underlying factors contribute to the high cost of medicinal cannabis in Australia, creating a complex pricing environment that disadvantages patients:
- Regulatory Compliance Requirements: The Therapeutic Goods Administration (TGA) has stringent rules for quality control, testing, and documentation. While vital for patient safety, these increase production and distribution costs, ultimately passed to patients. TGA fees, updated as of May 2025, and Office of Drug Control (ODC) cost recovery mechanisms for regulating medicinal cannabis further contribute to the financial burden on the supply chain [10], [11].
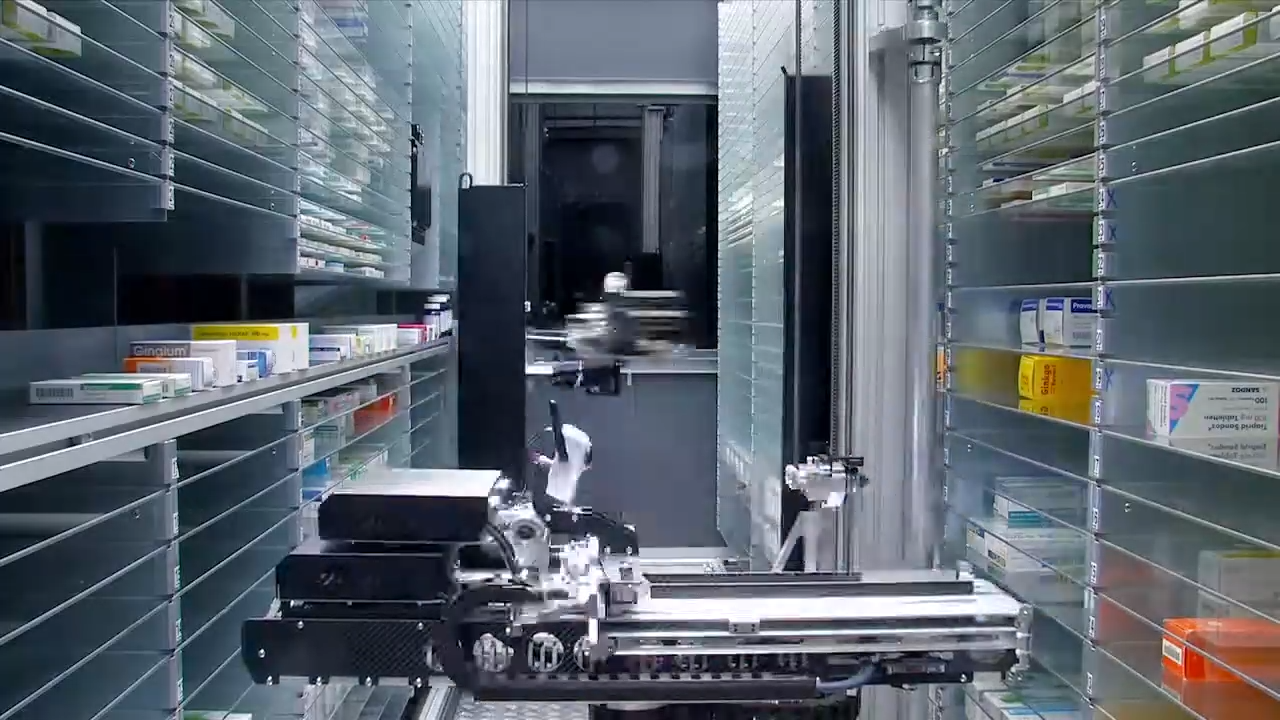
- Limited Market Competition and Retail Bottlenecks: The Australian medicinal cannabis market is still maturing. Industry analysts from Business of Cannabis project Australia will surpass AUD$1 billion in sales by the end of 2025, making it the largest medical cannabis market outside the U.S. [7]. Despite this growth and the emergence of more dedicated dispensaries – some even likened to "high-end boutiques" [8] – market fragmentation and distribution bottlenecks still inflate consumer prices. Efficient fulfillment infrastructure, such as that provided by dedicated medicinal cannabis pharmacies like Chronic Care Pharmacy, plays a crucial role in mitigating these distribution challenges by ensuring compliant, timely, and secure delivery of products to patients.
- Import and Supply Chain Costs: Many medicinal cannabis products sold in Australia are imported, incurring significant shipping, customs, and quarantine fees. While domestic production is growing, it has not yet reached a scale that would significantly reduce prices.
- Absence of PBS Subsidization: Unlike many other pharmaceutical products for chronic conditions, medicinal cannabis does not receive government funding through the PBS. Patients must bear the full commercial cost without the price protections that apply to other Schedule 8 medications.
These financial barriers significantly impact patient decisions about treatment, with many forced to choose between their medication and other essential expenses. This economic reality transitions directly into the second major barrier: the legal complexities surrounding medicinal cannabis use.
Drug-Driving Laws: A Legal Trap for Legitimate Patients
Zero-Tolerance Policies Create Practical Barriers
Beyond the financial challenges, another major obstacle for medicinal cannabis patients in Australia is the clash between their legal prescription status and state drug-driving laws. Most Australian states have zero-tolerance policies for THC in a driver's system, regardless of whether the driver is actually impaired. This legal framework punishes patients simply for the presence of THC metabolites, not for actual impairment.
This creates a situation where using legally prescribed medication can lead to criminal charges, effectively forcing patients into an impossible choice between their health and their mobility. Legal experts at Coutts Legal highlight that the current framework means patients face "potential legal consequences... even if they are using cannabis for medical purposes" [8].
Key Legal Issues:
- License loss: Patients can lose their driver's licenses even if using their prescribed medication as directed.
- Persistent detection: THC metabolites can be detected in saliva for hours or even days after use, long after any psychoactive effects have worn off.
- No impairment link: There is no direct link between detectable THC presence and actual driving impairment based on current testing methods.
- Impossible choice: Patients face a difficult decision: either forgo necessary medication to keep their driver's license, or use their medication and risk criminal prosecution for driving while legally medicated.
Tasmania's Alternative Approach
Tasmania is an exception to this strict approach, demonstrating that alternative models can balance patient rights with road safety. Tasmanian law allows medicinal cannabis patients to drive legally as long as they are not impaired at the time they are driving. This impairment-based model is similar to how other prescription medications that might affect driving, like opioids or benzodiazepines for chronic conditions, are handled.
The Tasmanian model recognizes that:
- Mobility is essential: Medicinal cannabis patients often need to drive to maintain employment and access healthcare.
- Presence does not mean impairment: Just having THC metabolites in the system does not automatically mean a driver is impaired.
- Responsible use is possible: Patients can use prescribed medications responsibly without being automatically treated as criminals.
- Impairment testing is key: Testing for actual impairment, rather than just presence, offers appropriate road safety protection.
This approach demonstrates a workable alternative that balances road safety concerns with patient rights and practical access to prescribed treatment, offering a blueprint for potential nationwide reform.
Impact on Patient Decision-Making
The threat of losing one's license significantly discourages people from using medicinal cannabis, creating real-world consequences that extend far beyond the courtroom:
- Employment Consequences: Many patients, especially in regional areas, need a driver's license for work. The risk of losing their license might seem greater than the potential health benefits, forcing patients to avoid treatment or stick with less effective traditional therapies.
- Healthcare Access: Patients in areas with limited public transport rely on driving to go to medical appointments, pick up prescriptions, and access essential services. Losing a license effectively cuts these patients off from the healthcare system.
- Treatment Adherence: Fear of random roadside drug testing might cause patients to miss doses, reduce how often they take their medication, or stop treatment entirely. This reduces the medication's effectiveness and defeats the purpose of legal prescription access.
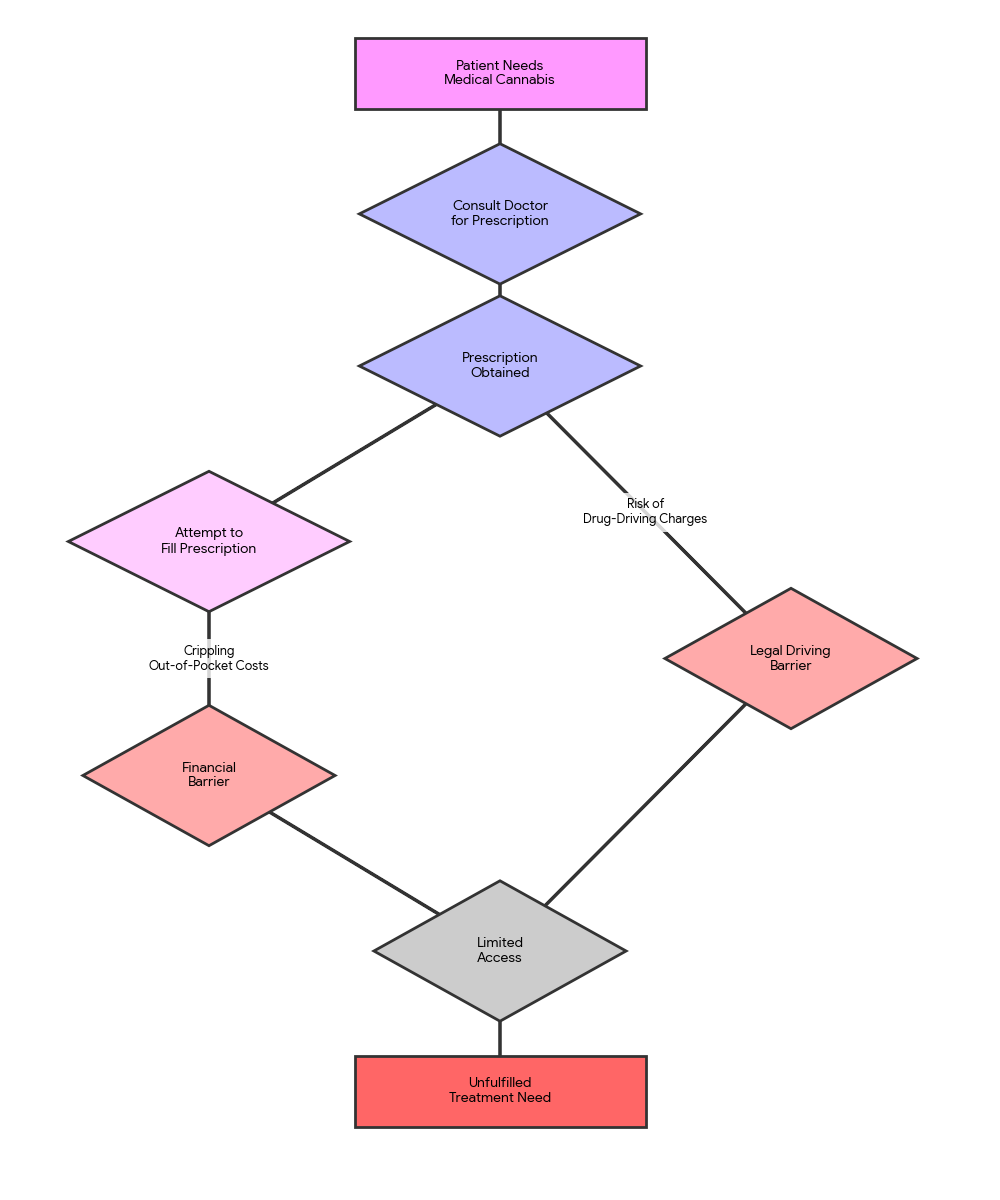
These combined financial and legal barriers create a complex navigation challenge for patients, as illustrated in the following flowchart.
Patient Journey with Medicinal Cannabis Access Barriers in Australia
Comparing Regulatory and Financial Models for Access
Addressing the multifaceted barriers to medicinal cannabis access requires diverse strategies. Understanding the strengths and limitations of different approaches helps stakeholders identify the most effective solutions for their specific situations. Below is a comparison of different models, highlighting their suitability for various stakeholders and desired outcomes.
Zero-Tolerance Drug Driving - Protecting road safety from all illicit drug use - Clear, unambiguous enforcement; Discourages recreational use - Penalizes legally prescribed patients; No link to actual impairment; Limits patient mobility - Current standard in most Australian states; ignores medical context.
Impairment-Based Drug Driving - Legally prescribed patients; Fair road safety - Protects patient rights; Focuses on actual impairment; Promotes mobility - Requires robust and reliable impairment testing methods; Public perception challenges for change - Tasmanian model; aligns with testing for other impairing prescription medications.
Full PBS Subsidization - Low-income patients; Equitable access - Drastically reduces patient costs; Increases access; Reduces financial toxicity - High government expenditure; Complex approval process for PBS inclusion - Ideal for making medicinal cannabis as accessible as other essential medicines; long-term policy goal.
Concession/Bulk-Billing Options - Vulnerable patient groups; Initial cost relief - Targeted financial relief; Easier to implement than full PBS - Still leaves significant out-of-pocket costs for many; Not a complete solution for high product costs - More immediate and politically feasible than full PBS inclusion; provides a necessary stepping stone for broader reform.
Optimised Pharmacy Fulfillment - Clinics, Telehealth Networks, Patients - Ensures compliant, efficient, and safe delivery of medications; Reduces dispensing errors; Streamlines patient access post-prescription. - Does not directly address product cost or legal frameworks; Requires investment in infrastructure. - Essential for reliable last-mile delivery and patient safety, as demonstrated by Chronic Care Pharmacy's operations.
Choose the approach if:
- You are a patient needing to drive: Advocate for an impairment-based drug-driving model to protect your mobility while legally medicated.
- You believe in equitable healthcare access: Support full PBS subsidization to ensure medicinal cannabis is affordable for all eligible patients, regardless of income.
- You seek immediate, practical financial relief for vulnerable patients: Push for concession/bulk-billing options to ease the initial financial burden on those most in need.
- You prioritize road safety based on actual capacity to drive: Champion impairment-based drug-driving policies that differentiate between presence and impairment.
While policy reform remains essential, practical infrastructure improvements can immediately enhance patient access within the current system.
The Role of Infrastructure in Addressing Access Barriers
While policy changes are crucial for solving both cost and legal issues, robust pharmaceutical infrastructure can significantly ease access challenges within the existing framework. Specialized fulfillment services play a vital role in ensuring that once patients overcome the financial and legal hurdles to obtain prescriptions, they can access their medications safely, reliably, and in compliance with stringent regulatory requirements.
Chronic Care Pharmacy in Brisbane operates as a leading medicinal cannabis fulfillment pharmacy. We specialize in the efficient and compliant dispensing of Schedule 8 medications, including medicinal cannabis products, within a sophisticated RTPM ecosystem designed for precision and safety.
As a TGA-compliant pharmacy warehousing facility, Chronic Care Pharmacy provides a suite of essential services:
- Clinical Safety Validation - PhD-led Command Centre, real-time script checks
- Same-Day Dispatch - Efficient processing for reduced patient wait times
- API Integration - Seamless connection with telehealth platforms
- Zero-Error Protocols - Strict S8 medication dispensing accuracy
- TGA-Compliant Warehousing - Secure storage meeting regulatory standards
For clinics and telehealth networks requiring reliable telehealth pharmacy fulfillment services, Chronic Care Pharmacy provides comprehensive solutions. Our PhD-led Clinical Command Centre, with its real-time script checks and zero-error protocols, directly mitigates prescriber liability and enhances clinical safety. We ensure efficient pharmacy logistics for clinics while maintaining expert-level risk analysis and compliance standards. This infrastructure approach improves fulfillment efficiency but cannot solve the underlying cost and legal barriers, which require legislative reform.
Understanding these infrastructure solutions alongside the need for policy reform provides a complete picture of what must change to improve patient access.
The Path Forward: Necessary Reforms
Addressing the current limitations requires a multi-faceted approach, combining financial and legal reforms to create meaningful change for patients.
Summary of Proposed Reforms
Financial Access Solutions
Meaningful financial reform must address the root cause of access inequality: the absence of government subsidization. Key proposals include:
- PBS Inclusion: The most effective reform would be to include medicinal cannabis products under PBS subsidization for approved chronic conditions. This would put medicinal cannabis on par with other Schedule 8 medications, reducing patient costs to standard co-payment levels.
- Bulk-Billing Options: Making bulk-billing more widely available for medicinal cannabis consultations would remove an initial barrier for low-income patients.
- Concession Pricing: Introducing concession card pricing for medicinal cannabis products would offer specific relief for pensioners, veterans, and other vulnerable patient groups.
Legal Framework Modernization
Legal reforms must align drug-driving laws with the reality of legal medicinal cannabis prescriptions:
- National Impairment-Based Testing: Adopting the Tasmanian model nationwide would bring drug-driving laws in line with the legality of medicinal cannabis prescriptions, protecting patients who use their medication responsibly.
- Prescription Registry Recognition: Creating a national prescription registry that law enforcement can verify during roadside testing would help distinguish legal patients from recreational users.
- Clear Legal Protections: Laws that explicitly protect prescribed medicinal cannabis patients from zero-tolerance policies would remove the current legal confusion.
These reforms, while substantial, are necessary to fulfill the promise made when medicinal cannabis was legalized in 2016. However, patients navigating the current system must also be aware of important clinical and regulatory considerations.
Important Considerations for Medicinal Cannabis Patients
Navigating medicinal cannabis treatment involves several important considerations that patients should discuss thoroughly with their healthcare providers:
- Product Variability: As the TGA's medicinal cannabis product list (updated September 2025) shows, products vary widely in cannabinoid content, quality, and efficacy [6]. It's crucial to consult with an authorised prescriber.
- Individual Response: Patient responses to medicinal cannabis can differ significantly based on physiology, condition, and product type.
- Limited Long-Term Research: While research is growing, long-term data on efficacy and safety, especially for specific conditions, is still developing.
- Potential Side Effects: Common side effects can include dizziness, fatigue, dry mouth, and changes in appetite. Serious interactions with other medications are possible.
- TGA Approval Status: Most medicinal cannabis products are "unapproved" therapeutic goods, meaning they have not undergone the full TGA evaluation process for safety, quality, and efficacy required for registered medicines. They are accessed via the Special Access Scheme (SAS) or Authorised Prescriber (AP) scheme [9].
- Disclaimer: This information is for general educational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.
Always read the label. Use only as directed. If symptoms persist, consult your healthcare professional.
Frequently Asked Questions (FAQs)
Q: How do I obtain a legal medicinal cannabis prescription in Australia?
A: Access generally requires consultation with a registered medical practitioner who is either an Authorised Prescriber or can apply to the TGA via the Special Access Scheme (SAS) for your specific condition. Telehealth services have made this process more accessible [2].
Q: Is medicinal cannabis covered by private health insurance or Medicare?
A: Currently, medicinal cannabis products are not subsidized by the Pharmaceutical Benefits Scheme (PBS), nor are they typically covered by Medicare. Some private health insurers may offer limited rebates for consultations but rarely for the products themselves.
Q: Can I grow my own medicinal cannabis for personal use in Australia?
A: No, under current federal and state laws, it remains illegal for individuals to cultivate cannabis, even if they hold a medicinal cannabis prescription.
Q: What conditions is medicinal cannabis commonly prescribed for?
A: Medicinal cannabis is prescribed for a range of conditions, including chronic pain, chemotherapy-induced nausea and vomiting, multiple sclerosis spasticity, epilepsy, and palliative care symptoms. Prescribers evaluate each case individually based on available evidence and patient needs [9].
Q: What are the drug-driving laws for medicinal cannabis patients in my state?
A: Most Australian states enforce zero-tolerance policies, meaning any detectable THC can result in penalties regardless of impairment. Tasmania is the exception, allowing medicinal cannabis patients to drive if not impaired. Always check your specific state's regulations and consider how this affects your treatment decisions.
Conclusion
Australian patients seeking relief from medicinal cannabis face a critical double challenge: crippling financial strain and pervasive legal vulnerability. Despite Australia's medicinal cannabis market rapidly approaching an astounding AUD$1 billion in annual sales by early 2026, the average patient still bears substantial, often prohibitive, out-of-pocket costs, historically averaging around $79.20 weekly. Coupled with strict, zero-tolerance drug-driving laws that pose the constant threat of license loss, countless eligible patients are either deterred from accessing or forced to discontinue vital treatment, despite holding legitimate prescriptions.
The persistent lack of PBS subsidization creates insurmountable cost barriers that unjustly penalize patients with chronic conditions—precisely those who stand to benefit most from medicinal cannabis therapy. The stark difference between restrictive state approaches and Tasmania's pragmatic, impairment-based model underscores the urgent need for change and demonstrates that better solutions are not only possible but already proven. Until comprehensive and decisive reforms address both financial barriers and glaring legal inconsistencies, the promise of medicinal cannabis access remains tragically unfulfilled for tens of thousands of Australian patients.
For prescribers and telehealth networks, ensuring safe and compliant patient care is paramount. Chronic Care Pharmacy offers specialized pharmacy logistics for clinics and schedule 8 medication dispensing pharmacy infrastructure, including a PhD-led Clinical Command Centre to safeguard against prescriber risk and optimize medicinal cannabis dispensary Australia services. Streamline your clinic's dispensing and enhance patient care today by partnering with a trusted fulfillment pharmacy.
Quick Steps for Navigating Medicinal Cannabis Access
- Consult a Qualified Prescriber: Seek an Authorised Prescriber or specialized clinic to discuss eligibility and obtain a legitimate prescription.
- Assess Financial Commitment: Understand all potential out-of-pocket costs, including consultations, product prices, and dispensing fees.
- Clarify Drug-Driving Laws: Inquire about your state or territory's specific drug-driving policies regarding medicinal cannabis to avoid legal repercussions.
- Explore Patient Support: Connect with patient advocacy groups or online communities for shared experiences and information on reform efforts.
- Choose a Reliable Pharmacy Partner: Ensure your chosen pharmacy specializes in Schedule 8 medicinal cannabis fulfillment for compliant and efficient medication access.
Patient Readiness Checklist
- Have you thoroughly discussed all medicinal cannabis treatment options and potential side effects with your healthcare professional?
- Are you fully aware of the total financial commitment required for your prescribed medicinal cannabis, including product and dispensing costs?
- Do you understand the drug-driving laws specific to your state/territory and their implications for your medication use?
- Have you identified a reliable, TGA-compliant pharmacy that can efficiently dispense your Schedule 8 medicinal cannabis prescription?
- Have you considered alternative transportation methods or adjusted your daily routines if driving restrictions apply to your medication use?
Snippet for Clinics: Ensure seamless patient care by partnering with a TGA-compliant fulfillment pharmacy specializing in Schedule 8 medications. Focus on clinical excellence; let your pharmacy partner handle the logistics and mitigate prescriber risk.
Citations
- [1] https://www.medio.com.au/cheap-medical-cannabis
- [2] https://cannaaidmedical.com.au/how-much-does-medical-cannabis-cost-in-australia
- [3] https://sydneykush.com/medical-marijuana-australia-cost
- [4] https://pmc.ncbi.nlm.nih.gov/articles/PMC9854313
- [5] https://brotherkitchen.com.au/blog/breaking-down-medical-cannabis-cost-in-australia
- [6] https://businessofcannabis.com/high-thc-leads-growth-as-australia-tightens-tga-prescribing-rules
- [7] https://www.tga.gov.au/products/unapproved-therapeutic-goods/medicinal-cannabis-hub/medicinal-cannabis-guidance-documents/guidance-use-medicinal-cannabis-australia-overview
- [8] https://couttslegal.com.au/blog/what-you-need-to-know-about-prescribed-cannabis-and-driving
- [9] https://www.imarcgroup.com/australia-medical-cannabis-market
- [10] https://www.smh.com.au/business/entrepreneurship/medicinal-cannabis-dispensaries-like-aesop-the-rise-of-high-street-weed-boutiques-20260121-p5nvwa.html
- [11] https://www.odc.gov.au/resources/publications/cost-recovery-implementation-statement-cris-regulation-medicinal-cannabis
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Partner with our medicinal cannabis fulfillment pharmacy in Australia for same-day dispatch and clinical oversight that protects your clinic.

The National Data Exchange tracks supply, not refusal. We expose the ‘Refusal Loophole’ – a systemic blind spot where clinical safety interventions vanish. Discover how ‘Jurisdictional Arbitrage’ weaponises this data gap against your prescribing authority.

Discover Australia's medical cannabis market: balancing GMP quality standards, product diversity, and therapeutic integrity amid rapid growth and regulatory challenges.
%20(1).svg)
