The 'Postcode Lottery': How Geography and Income Create a Two-Tier System for Medicinal Cannabis Access
Discover Australia's 'postcode lottery' in medicinal cannabis access, where geography and income create barriers, and learn solutions for equitable treatment.

The 'Postcode Lottery': How Geography and Income Create a Two-Tier System for Medicinal Cannabis Access
As of January 2026, Australia's medicinal cannabis program aimed to provide fair access to patients with qualifying conditions. However, a significant inequitable problem persists, creating a stark two-tier system: where individuals live and their income level can profoundly influence their ability to access treatment. Despite federal frameworks established by the Therapeutic Goods Administration (TGA) [1], a clear disparity is evident. This disparity strongly indicates that urban areas with higher wealth often facilitate easier access, while rural and lower-income Australians face substantial barriers.
This 'postcode lottery' is a systemic challenge, placing patients in difficult situations. They might need to relocate from family and community, go without prescribed medication, or seek unregulated sources. For telehealth networks and clinics prescribing medicinal cannabis, understanding these systemic barriers is crucial—not only for patient outcomes but also for ensuring that clinical infrastructure does not accidentally increase inequality. Chronic Care Pharmacy Brisbane recognizes these challenges and provides solutions designed to bridge the gap between patient need and access.
The Geography Trap: Rural Australia's Access Disparities
Living in regional or remote Australia creates numerous barriers to medicinal cannabis access that patients in major cities may not face. The reason is straightforward yet consequential: prescribers, specialized pharmacies, and consultation services often concentrate in urban centers, leaving rural populations isolated from the entire care pathway. While specific nationwide statistics on the exact urban-to-rural ratio of Authorised Prescribers are not always publicly available, TGA data on prescriber approvals by state consistently shows that a large number of medical professionals with the necessary expertise work in major capital cities [9]. This reflects a broader trend in medical specialization, with research indicating that rural living remains a significant barrier for patients seeking medicinal cannabis, despite telehealth's partial mitigation of geographical hurdles [8] [8].
The 'Cannabis Refugee' Phenomenon
Research into patient barriers indicates that some Australians have taken the significant step of moving to gain access to medicinal cannabis, a phenomenon described as becoming 'cannabis refugees' [2]. These patients may need to leave established social networks, jobs, and family connections simply to live within practical reach of prescribers and fulfillment services.
The concentration of services in certain areas creates several problems:
- Limited prescriber availability: Authorised Prescribers and clinicians experienced with medicinal cannabis primarily work in Brisbane, Sydney, and Melbourne.
- Pharmacy access gaps: Specialist pharmacies that can handle Schedule 8 (S8) medicinal cannabis may be rare outside capital cities.
- Travel burden: Patients can face multi-hour journeys for initial consultations and follow-up appointments, involving accommodation and transport costs that city patients might avoid.
Why Distance Multiplies Cost
Geographic isolation does not only add inconvenience; it significantly increases the total cost of access. A rural patient might face:
- Travel expenses: Typically $200–$400 in fuel and accommodation for consultation travel.
- Lost wages: From time away from work.
- Repeat travel: For follow-up appointments when telehealth is not sufficient.
- Delayed medication access: If local pharmacies cannot fill prescriptions.
For patients managing chronic conditions that require ongoing prescriptions, these costs recur monthly or quarterly, creating a considerable cumulative financial burden that city patients may not experience to the same extent.
The Income Barrier: When Cost Dictates Treatment
Beyond geography, the financial burden of medicinal cannabis access has 'remained largely unchanged' since the program started—a persistent barrier that consistently excludes lower socioeconomic populations [3]. Unlike many therapeutic goods on the Pharmaceutical Benefits Scheme (PBS), medicinal cannabis products remain almost entirely out-of-pocket expenses.
The Comprehensive Cost Structure
The real financial barrier involves more than just prescription costs. Consider the complete expense profile:
Cost ComponentTypical RangeFrequencyInitial specialist consultation$150–$350One-timeTGA approval (SAS pathway)$0–$150Per prescriptionMedicinal cannabis product$200–$600MonthlyFollow-up consultations$80–$200QuarterlyPharmacy dispensing fees$10–$30Per prescription
For a patient on a stable treatment plan, annual costs can often exceed $3,000–$5,000. This is prohibitively expensive for many Australians, especially those with chronic conditions that limit their ability to work.
Disproportionate Impact on Vulnerable Populations
The financial barrier creates selection pressure that unfairly affects populations who might benefit most from medicinal cannabis access:
- Chronic pain patients: Who may have reduced ability to work due to their condition.
- Pensioners and retirees: Who are on fixed incomes without additional resources for healthcare.
- Regional workers: In industries without employer health coverage.
- Single parents: Who are managing healthcare costs for their children.
This socioeconomic filter does not reflect clinical need. Instead, it reflects the ability to pay, creating a system where financial capacity dictates treatment access rather than medical necessity.
The Unregulated Path: Return to Illicit Markets
When legal pathways become financially or geographically prohibitive, patients face a difficult choice: manage without treatment or seek cannabis through illicit channels. Evidence suggests that cost barriers frequently lead patients to seek alternative, unregulated sources [4], which directly undermines the therapeutic framework established by the TGA.
Why Patients May Forego Legitimate Access
The decision-making process is heavily influenced by cost comparisons. A patient paying $400–$600 monthly for legal medicinal cannabis might find similar quantities illicitly for $200–$300. For someone on a disability pension or managing a chronic condition with limited income, this cost difference can be impossible to ignore.
This shift to unregulated sources creates several clinical risks:
- Uncontrolled product quality: Illicit cannabis typically lacks the quality controls and testing required for TGA-approved products.
- Inconsistent cannabinoid profiles: Patients lose the standardization that makes medicinal cannabis treatment predictable and dose-adjustable.
- Loss of clinical oversight: Prescribers cannot monitor treatment effectiveness or adjust dosing if patients do not disclose their use of unregulated products.
- Legal exposure: Patients risk criminal penalties for possession, which can worsen existing health vulnerabilities.
Prescriber Considerations in the Affordability Gap
For telehealth networks and clinics, patient affordability barriers represent a critical clinical consideration. When patients express concerns about cost, prescribers must navigate difficult conversations about access limitations, yet many lack the infrastructure or tools to support patients through these financial barriers.
This is where specialized fulfillment infrastructure becomes important. Chronic Care Pharmacy Brisbane operates as a business-to-business (B2B) pharmacy logistics partner positioned to help overcome the retail bottleneck that often hinders patient access. By employing a PhD-led Clinical Command Centre for TGA-compliant warehousing and zero-error dispensing, it actively reduces friction in the fulfillment process. Its specialized B2B infrastructure addresses geographic barriers in the cost equation by tackling pharmacy access gaps through national dispatch and ensuring same-day fulfillment for approved prescriptions. This positions it as a B2B partner for telehealth networks, contrasting sharply with direct-to-consumer pharmacy models (e.g., Chemist2U) that focus solely on individual patient transactions.
The International Context: Australia Is Not Alone
The 'postcode lottery' phenomenon extends beyond Australia's borders, reflecting systematic patterns in medicinal cannabis programs globally. International research reveals similar geographic and socioeconomic disparities across multiple jurisdictions.
Geographic Concentration in New York State
A study examining New York's medical cannabis program found significant disparities in service availability based on neighborhood characteristics [5]. Dispensaries and medical cannabis services often concentrated in affluent urban areas, while neighborhoods with higher poverty rates and minority populations had substantially reduced access—a pattern remarkably similar to Australia's experience.
Telemedicine as a Partial Solution
Recent geospatial research suggests that virtual care can help reduce socioeconomic disparities in medical cannabis access [6]. Telemedicine can address the travel barrier for consultations, allowing rural patients to access experienced prescribers without needing to relocate. However, telehealth alone cannot solve the affordability crisis—it primarily addresses one barrier in a multi-layered access problem.
The UK's Similar Challenges
The United Kingdom's medicinal cannabis program demonstrates similarly challenging 'postcode lottery' issues. Despite legislative changes in 2018, only 49 out of 106 Clinical Commissioning Groups routinely offer cannabis-based medicines [7], leaving patients dependent on arbitrary geographic boundaries for access to treatments like Sativex for multiple sclerosis.
One affected couple in Hull described the system as 'cruel', denied access to potentially life-changing medication solely based on their postcode [7]. The situation presents clear parallels to Australia's experience: federal frameworks may exist, but implementation creates geographic barriers that undermine equitable access.
What Perpetuates the Two-Tier System
The persistence of these access barriers is not accidental—it reflects policy choices and infrastructure gaps that compound geographic and economic disadvantages. Addressing the 'postcode lottery' requires understanding the structural factors that maintain it.
Lack of PBS Coverage
Unlike most therapeutic goods, medicinal cannabis remains excluded from the Pharmaceutical Benefits Scheme (PBS). This single policy decision transforms medicinal cannabis from an affordable prescription medicine into a prohibitive healthcare expense, severely excluding lower-income populations who could benefit most from subsidized access.
Prescriber Concentration
The Authorised Prescriber pathway requires specific TGA approval and clinical expertise that is highly concentrated in metropolitan teaching hospitals and specialist clinics. Regional General Practitioners (GPs) often lack either the authorization or confidence to prescribe medicinal cannabis, necessitating rural patients to seek distant urban specialists. TGA data on Authorised Prescribers, while not detailing urban/rural distribution, consistently shows higher approval rates in states with larger urban populations, reinforcing the concentration effect [9].
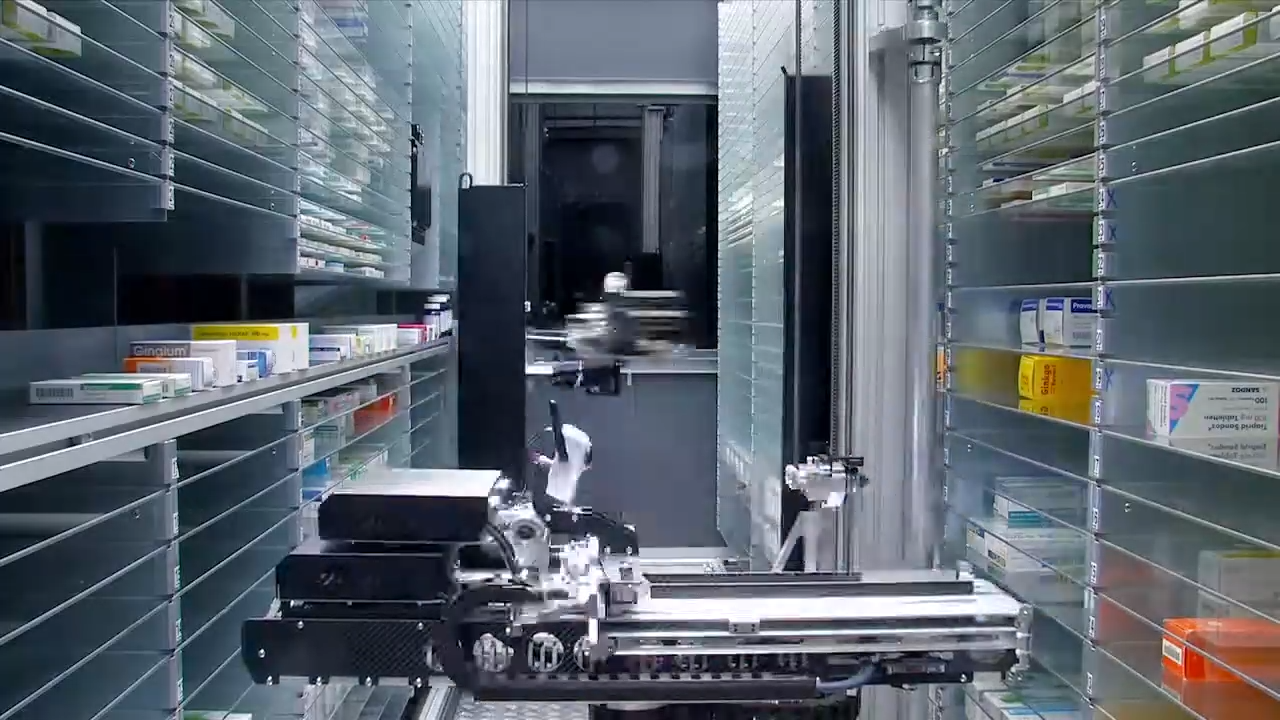
Pharmacy Capability Gaps
Standard community pharmacies often face a significant retail bottleneck, lacking the specialized refrigerated storage, Schedule 8 (S8) handling protocols, and robust stock management systems required for medicinal cannabis fulfillment. This creates "pharmacy deserts" in regional areas, where even patients with valid prescriptions struggle to access their medication locally.
Specialized fulfillment infrastructure can address this gap. Chronic Care Pharmacy Brisbane's PhD-led Clinical Command Centre for fulfillment ensures that telehealth prescriptions can reach patients nationwide through TGA-compliant warehousing and real-time clinical safety validation. By operating as a strategic B2B infrastructure partner for telehealth networks rather than a direct-to-consumer pharmacy, such services aim to reduce the pharmacy availability barrier, though they do not fully address the affordability crisis.
Navigating Access: A Comparison of Pathways
Understanding the different legitimate pathways for medicinal cannabis access is crucial for both patients and healthcare providers. Each model offers distinct advantages and disadvantages in tackling geographic and financial barriers.
OptionSuitable ForProsConsNotes1. In-Person Clinic & Local Community PharmacyPatients in major urban centers seeking direct physical interaction with prescribers and local pharmacy pickup.Direct physical examination; potential for immediate medication if pharmacy is local and stocks.High geographic barrier for rural patients; reliance on a local pharmacy's capability and stock; travel costs/time for follow-ups; potential for higher consultation fees.Traditional model, most effective in densely populated areas.2. Telehealth Consultation & Standard Local PharmacyPatients in regional areas seeking remote consultation but can access a nearby, capable community pharmacy.Addresses consultation travel barrier; greater access to specialist prescribers regardless of location.Still relies on local pharmacy's stock and S8 handling capabilities; significant geographic barrier if no local capable pharmacy; potential for delays if pharmacy needs to order in.Reduces initial consultation travel, but fulfillment remains a challenge if local infrastructure is lacking.3. Telehealth Consultation & Specialized National Fulfillment (e.g., Chronic Care Pharmacy)Patients nationwide, especially in regional/remote areas, prioritizing consistent access and compliant fulfillment.Addresses both consultation travel and pharmacy access gaps nationwide; TGA-compliant warehousing; zero-error dispensing; rapid dispatch.Does not directly address the affordability barrier (product cost); requires patient comfort with remote consultation and medication delivery.Designed for seamless patient access and clinical compliance across Australia, overcoming the "retail bottleneck" for telehealth networks.
Choose Your Pathway Based On:
- Proximity to Specialist Clinics & Pharmacies: Choose Option 1 if you live in a major city with easy access to both specialized prescribers and capable pharmacies.
- Need for Remote Consultation but Some Local Pharmacy Support: Choose Option 2 if you need to consult remotely but have a reliable, capable local pharmacy that can fulfill medicinal cannabis prescriptions.
- Location in Regional/Remote Australia or Need for Guaranteed Compliant Fulfillment: Choose Option 3 if geographic barriers to specialized pharmacy access are significant, or if your prescriber requires a robust, compliant fulfillment partner with national reach.
- Cost Sensitivity (Product vs. Access): All options incur product costs; Option 3 aims to minimize access-related costs (travel, delays) through efficient national delivery.
Clinical Implications for Prescribers
For medical practitioners prescribing medicinal cannabis through telehealth platforms, understanding these access barriers is clinically imperative. Patient adherence depends not only on treatment efficacy but also on whether patients can afford and physically obtain their prescribed medication.
Questions Prescribers Should Consider
During consultation and follow-up, practitioners should assess:
- Geographic accessibility: Can the patient physically access a pharmacy capable of fulfilling medicinal cannabis prescriptions?
- Financial sustainability: Can the patient afford ongoing treatment costs, or will they likely discontinue medication due to expense?
- Support systems: Does the patient have family or community support that might help with travel or cost burdens?
- Alternative pathway awareness: Is the patient aware of patient assistance programs, bulk-buying options, or telehealth consultation discounts?
The Role of Infrastructure in Equity
While prescribers cannot solve systemic funding gaps, choosing fulfillment partners that minimize access friction is a critical consideration. Services offering:
- National same-day dispatch to address geographic pharmacy gaps.
- API integration for seamless prescription flow without patient coordination burden.
- Clinical oversight through doctorate-level pharmacist review to identify potential issues before they reach patients.
These infrastructure choices do not address affordability directly, but they are crucial for eliminating the compounding effect where geographic barriers increase financial strain through travel costs and delays.
Policy Reforms Needed to Address the Two-Tier System
The two-tier system is not inevitable—it reflects policy choices that have prioritized restriction over access. Meaningful reform requires structural changes at multiple levels of the medicinal cannabis framework.
PBS Inclusion for High-Need Populations
Targeted PBS subsidy for patients with qualifying chronic conditions would significantly reduce the financial barrier. Even partial subsidy (e.g., reducing cost to $42.70 per prescription for concession card holders) would dramatically improve access for vulnerable populations who currently cannot afford treatment.
Regional Prescriber Training Programs
Expanding the number of Authorised Prescribers in regional Australia through targeted training and mentorship programs would directly address the geographic concentration issue. This would reduce the need for patients to seek distant urban specialists and help distribute clinical expertise more equitably across the country.
Pharmacy Capability Grants
Government funding to assist regional pharmacies in establishing TGA-compliant Schedule 8 (S8) storage and handling systems would expand the fulfillment network beyond capital cities, creating local access points that reduce travel burdens and associated costs.
Telemedicine Pathway Standardization
Establishing clear, standardized telehealth pathways for medicinal cannabis consultation and follow-up would formalize virtual care as an essential access solution, directly reducing the 'cannabis refugee' phenomenon by enabling patients to remain in their communities while accessing specialist care.
Conclusion: Access as a Clinical Outcome
The 'postcode lottery' in medicinal cannabis access reveals a fundamental truth: access itself is a clinical outcome. The most effective treatment offers no therapeutic benefit if patients cannot afford or physically obtain it.
For telehealth networks and prescribers, addressing access barriers requires both advocacy for systemic reform and strategic infrastructure choices that minimize geographic and logistical friction. While individual clinical practices cannot solve Australia's affordability crisis, they can strategically partner with fulfillment services that aim to reduce unnecessary barriers. Chronic Care Pharmacy Brisbane provides telehealth pharmacy fulfillment services that address pharmacy availability as a barrier through national dispatch, TGA-compliant warehousing, and zero-error clinical validation. By operating as business-to-business (B2B) infrastructure for telehealth networks, such services effectively address the geographic component of the access crisis, though broader policy reform remains essential for true equity.
Always read the label. Use only as directed. If symptoms persist, consult your healthcare professional.
For telehealth networks seeking to minimize patient access barriers through specialized fulfillment infrastructure, contact Chronic Care Pharmacy to discuss clinical partnership options.
Frequently Asked Questions (FAQs)
What is the "postcode lottery" for medicinal cannabis access in Australia?
The "postcode lottery" describes how a patient's geographic location and income significantly influence their ability to access medicinal cannabis in Australia, creating a two-tier system where metropolitan and wealthier individuals often have better access than rural and lower-income Australians.
How does geography create barriers to medicinal cannabis access?
Geographic barriers arise when prescribers and specialized pharmacies concentrate in urban centers, isolating rural populations. This leads to limited prescriber availability, pharmacy access gaps, and significant travel burdens for regional patients seeking treatment.
What is the "cannabis refugee" phenomenon?
The "cannabis refugee" phenomenon refers to patients who relocate, often to urban areas, to gain access to medicinal cannabis due to a lack of local prescribers and fulfillment services in their original location.
Why is medicinal cannabis often expensive in Australia?
Medicinal cannabis is expensive primarily due to its exclusion from the Pharmaceutical Benefits Scheme (PBS), making it an entirely out-of-pocket expense. Total costs typically include initial consultations, TGA approvals, product costs, follow-up appointments, and dispensing fees, often exceeding $3,000–$5,000 annually.
What are the risks of patients returning to illicit markets for medicinal cannabis?
When legitimate access is costly or difficult, patients may seek unregulated sources. This poses significant risks including uncontrolled product quality, inconsistent cannabinoid profiles, loss of clinical oversight, and potential legal exposure.
How does Chronic Care Pharmacy help address medicinal cannabis access barriers?
Chronic Care Pharmacy Brisbane acts as a business-to-business (B2B) pharmacy logistics partner, providing TGA-compliant warehousing and zero-error dispensing. It minimizes geographic barriers by offering national dispatch and same-day fulfillment to ensure telehealth prescriptions reach patients efficiently, effectively overcoming the retail bottleneck faced by many traditional pharmacies.
What policy changes could improve medicinal cannabis access in Australia?
Key policy changes include PBS inclusion for high-need populations, expanded regional prescriber training programs, government grants for regional pharmacy capabilities, and standardized telehealth pathways. These reforms could foster a more equitable system.
How does telehealth impact access to medicinal cannabis?
Telehealth can partially reduce socioeconomic disparities by addressing the travel barrier for consultations, enabling rural patients to access experienced prescribers remotely. However, it does not fully address the underlying affordability crisis, which requires broader policy reform.
Citations
- [1] https://www.tga.gov.au/products/unapproved-therapeutic-goods/medicinal-cannabis/access-pathways
- [2] https://www.medicinalcannabis.nsw.gov.au/patients/access
- [3] https://www.tga.gov.au/accessing-medicinal-cannabis-patient
- [4] https://www.cannabistrades.org/articles/cta-responds-to-home-office-call-for-evidence-on-medicinal-cannabis
- [5] https://www.bbc.com/news/uk-england-humber-58256351
- [6] https://pmc.ncbi.nlm.nih.gov/articles/PMC8988426
- [7] https://www.medrxiv.org/content/10.1101/2024.12.05.24318514v1.full
- [8] https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0277355
- [9] https://www1.racgp.org.au/ajgp/2025/march/exploring-access-to-medicinal-cannabis-through-gen
Links
Everything you need to scale your clinic, without the retail overhead.
Other article

Discover how Australia's medicinal cannabis program is reshaping drug regulation, bypassing traditional approvals and setting precedents for psychedelics and unapproved medicines.

The National Data Exchange tracks supply, not refusal. We expose the ‘Refusal Loophole’ – a systemic blind spot where clinical safety interventions vanish. Discover how ‘Jurisdictional Arbitrage’ weaponises this data gap against your prescribing authority.

Discover how medication packaging systems safeguard patients, ensure TGA compliance, and boost efficiency in chronic care.
%20(1).svg)
